At an altitude of 30,000 feet, the healthcare reform objectives that link financial incentives to performance shine brightly. There are no protesting voices calling for poor outcomes, more medical errors or higher costs.
At an altitude of 30,000 feet, the healthcare reform objectives that link financial incentives to performance shine brightly. There are no protesting voices calling for poor outcomes, more medical errors or higher costs.
 At an altitude of 30,000 feet, the healthcare reform objectives that link financial incentives to performance shine brightly. There are no protesting voices calling for poor outcomes, more medical errors or higher costs.
At an altitude of 30,000 feet, the healthcare reform objectives that link financial incentives to performance shine brightly. There are no protesting voices calling for poor outcomes, more medical errors or higher costs.
Taking a playbook page from the corporate world, financial incentives and penalties are intended to drive performance improvements in healthcare delivery. But it’s reasonable to wonder how well big business theory—manufacturing thousands of new automobiles, for example—compares to the infinite variables, personal and one-to-one practice of medical arts.
And, while the goals are admirable, physicians, hospitals, medical groups and other healthcare providers question the validity of the standardized tools that are supposed to measure and reflect quality and efficiency.
A definitive report as to success or failure is somewhere down the road—along with how the nation’s Affordable Care Act eventually plays out in the real world. But related indicators show mixed results at best. Pay-for-performance doesn’t seem to make for better doctors or better outcomes.
- Often cited is a pay-for-performance study appearing in the New England Journal of Medicine titled, The Long-Term Effect of Premier Pay for Performance on Patient Outcomes. The comparison between hospitals with and without performance incentives concluded: “We found no evidence that the largest hospital-based pay-for-performance program led to a decrease in 30-day mortality.” N Engl J Med 2012; 366:1606-1615
- A study in the UK’s single-payer National Health System provided a large financial incentive for general practitioners achieving high quality care measures for patients with hypertension and other diseases. “Conclusions: Good quality of care for hypertension was stable or improving before pay for performance was introduced. Pay for performance had no discernible effects on processes of care or on hypertension related clinical outcomes.” BMJ 2011;342:d108
So… Does “pay or penalty” motivate people?
Author and lecturer Dan Pink has a revealing talk titled The Surprising Truth About What Motivates Us. He observes that “carrot or stick” motivators are not always effective, and that people “are not as endlessly manipulable and predictable as you would think.”
Take ten minutes to watch the delightful animated version of his presentation (link below). It illustrates what many academic studies show about the concept of reward and punishment as motivation tools, and what actually works.
A study at MIT—having to do with human motivation and not about healthcare directly—studied the typical organizational scheme of rewarding top performers and ignoring bottom performers. Findings included:
- As long as the task involved only mechanical skill, bonuses work as expected; but
- Once the task called for cognitive skill, reward led to poorer performance.
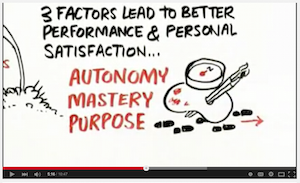
Academic studies appear to agree that money is not always a motivator, and that there are three factors that lead to better performance and personal satisfaction. Perhaps, not surprisingly, these three factors all resonate with medical professionals:
- Autonomy – the desire to be self-directed
- Mastery and Challenge – the urge to improve and make a contribution
- Purpose – companies with a higher purpose flourish
It remains to be seen how effectively healthcare’s present-day, pay-for-performance system will drive the intended improvements, or make better doctors and outcomes.
Daniel Pink’s RSA presentation concludes, however, that if business models can get past the carrot and stick ideology, and look at the science, society can build better organizations with the promise of building a better world.
For more about the surprising truth about what motivates us, watch the animated version here.