We’ll have to get to know patients, their needs; then build a care system around them.
We’ll have to get to know patients, their needs; then build a care system around them.
It may be hard to imagine a healthcare system tailored to address individual patient needs. Yet the healthcare system designed to treat conditions and provide patient services in the United States is not delivering the desired outcomes.
 We’ll have to get to know patients, their needs; then build a care system around them.
We’ll have to get to know patients, their needs; then build a care system around them.
It may be hard to imagine a healthcare system tailored to address individual patient needs. Yet the healthcare system designed to treat conditions and provide patient services in the United States is not delivering the desired outcomes.
In a recent study of healthcare in 11 countries by The Commonwealth Fund, the United States was ranked the highest in cost at $8,508 per person and last in overall performance. The United Kingdom was ranked #1 in overall performance and spent only $3,405 per person. The United States ranked last in efficiency (e.g., administrative costs), equity (e.g, variations such as socioeconomic status) and healthy lives (e.g., infant mortality, life expectancy).
Yet 800,000 international patients visit the United States each year for the innovative high quality care. If the “treatment of conditions” and “patient services” are already high quality, improving them may not have a major impact on the overall performance of the healthcare system.
Improvement is more likely to come from holistic approach to patients and their overall health. For the 5% of people that consume 50% of healthcare costs, a holistic approach is critical. The approach would include understanding and addressing the needs of patients that have 20 or more Emergency Room visits per year, rather than just providing great service each time in the cycle. Yet it would require revisions to the reimbursement system that only pays healthcare providers for “treatment of conditions” and “patient services”.
The third transformational wave of new reimbursement models (“covered lives” and “bundles”) may offer the opportunity to evolve toward overall patient outcomes. It would require getting to know patients better. It would require understanding more about the patient’s non clinical determinants that affect their clinical outcomes. This new patient information may not have been collected in the past as there was little that could be done with it. It could be that a patient with heart failure has no air conditioner at home or needs a nutritional hot meal each day. While there is no reimbursement for air conditioners or Meals on Wheels, paying for these could generate significant savings by avoiding ER visits or hospitalizations.
The mission of the new reimbursement models is to improve overall patient outcomes rather than just paying to treat each condition and to provide healthcare services. While the mission is essentially the same as previous waves, we are at a different place in transparency, technology and information.
To improve overall patient outcomes, we may be soon filling out forms (hopefully there’s an app for that) in the physician offices to help them understand the following:
What functional limitations do you have?
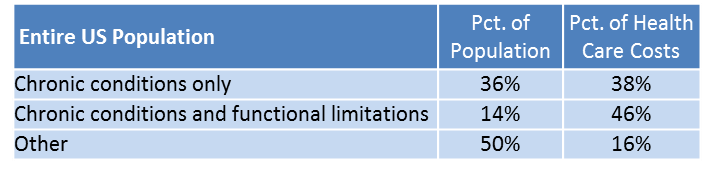
Patients with a combination of chronic conditions and functional limitations consume almost half of US healthcare spending.
Patient’s medical records may not record functional limitations as it may not be required to treat a condition or to bill for the patient service. If it is documented, it may be in a hand written note that may not be actionable. Functional limitations change, so even if it is in the medical record it may not be current.
Are your medical records accurate? Have we missed something?
A study has demonstrated that diagnoses that are missed, incorrect or delayed are believed to affect 10 to 20 percent of medical cases. A missing diagnosis can be critical in understanding the patient. Just 61% of Medicare’s quadriplegia beneficiaries had the diagnosis of quadriplegia reported in their medical record in the past 12 months.
How do you feel about your health status? What behaviors may be diminishing your overall health?
A recent study demonstrated an alternative method for determining future healthcare costs. Self-perception of physical health, smoking status and other answers were more effective at predicting future healthcare costs than the risk adjusted methods used by Medicare and health plans. Again, it’s information that is not required today to bill for healthcare services.
What barriers are preventing you from improving your overall health?
Patient barriers insight may only come from extensive dialog and developing trust with the patient. They include access to a physician or food, coordination of care activities, care decision making, a caregiver providing emotional and physical support, not appropriately monitoring conditions, financial constraints, home issues, not having an optimal medication list and understanding the instructions, access to mental health providers, nutrition, psychosocial issues, self-care capabilities, transportation and feeling a sense of purpose and meaning.
Can you tell us more about yourself?
While we ask our healthcare system to address the overall patient’s health, medical care represents only 10%-20% of the determinants of health outcomes. This is based on a review of several studies that show that behaviors, social circumstances, environment , genetics and stress impact as much as 90% of the health outcomes.
We may know someone we are afraid to ask, how are you feeling? To improve the overall health outcomes, we are going to have to get comfortable asking often and listening. We will also need to be able to justify the cost of interventions (see E interventions) not reimbursed today (like air conditioners and Meals on Wheels) to improve the overall patient outcomes and cost.