As part of the newly forming Health IT community in Seattle, the Unversity of Washington and the Washington Biotechnology and Biomedical Association have partnered on the “Health Innovator’s Collaborative,” which launched with a series of seminars on how the coming changes in US healthcare affect organizations and innovation.
As part of the newly forming Health IT community in Seattle, the Unversity of Washington and the Washington Biotechnology and Biomedical Association have partnered on the “Health Innovator’s Collaborative,” which launched with a series of seminars on how the coming changes in US healthcare affect organizations and innovation.
 This past Tuesday, I attended a talk by Paul Ramsey, MD, and CEO of University of Washington Medicine, entitled “The Transformation of Healthcare: Forces, Directions and Implications.” Despite this lofty title, Dr. Ramsey focused on the nuts and bolts of the new Affordable Care Act (ACA) with specific examples of how UW Medicine is becoming an Accountable Care Organization (ACO).
This past Tuesday, I attended a talk by Paul Ramsey, MD, and CEO of University of Washington Medicine, entitled “The Transformation of Healthcare: Forces, Directions and Implications.” Despite this lofty title, Dr. Ramsey focused on the nuts and bolts of the new Affordable Care Act (ACA) with specific examples of how UW Medicine is becoming an Accountable Care Organization (ACO).
First off, Dr. Ramsey started with some definitions of the goals of the Affordable Care Act and Accountable Care Organizations. When asked if the ACA is having a profound effect, he stated that regardless of any other measures, the number of individuals who are now insured is significant. Harborview Medical Center, a member of the UW Medicine System that covers a diverse and often low-income population, has already seen a 2% decrease in patients without coverage.
What was striking about the session was Dr. Ramsey’s clear conviction that while the ACA is morally just (we need to stop pricing people out of healthcare) organizations becoming ACOs were currently doing it because it makes human sense, while not currently financial sense. The reason it doesn’t currently make financial sense is that the first ACO contracts between payers and providers are still in negotiation and in the switch between reimbursements for procedures to reimbursement for outcomes providers initially see lower revenues as they decrease the number of unnecessary procedures. In the long run, this is mitigated by getting the right care to patients and by managing population health in addition to individual health
The triple aim of the ACA is to improve experiences for individuals, improve overall population health, and reduce the cost of care: lofty but extremely important goals. While managed care and HMOs were supposed to do this in the 90s, their main failure was having the primary care physician as the gatekeeper to all other services. This did not guarantee that the patient received the best and most cost effective care. Dr. Ramsey contrasted this to the goals of an ACO, where a patient might call a nurse hotline and be referred to emergency, their primary care physician, or receives an e-care visit, depending on which was best for the patient and most cost effective in the long run.
When asked if this model was a capitated model, Dr. Ramsey said yes, but at a population level, and that is why the current negotiations between payers and providers are so important. Providers are choosing which measures they will be held accountable for in their first year as an ACO. UW Medicine is choosing seven disease management measures, three health status and screening measures, and number of caesarian sections, which is apparently a hot button measure for CMS. Because all measures will not be implemented immediately UW Medicine will spend some time transitioning between models, however, this does not mean they won’t continue to improve care in all areas. He cited his own recent experience as a cataract patient at UW Medicine as of an example where high quality outcomes, patient care, and cost-effectiveness were combined.
As a guide for these types of measures, and as an example of the medical profession taking on best practices regardless of financial incentives, Dr. Ramsey cited http://www.choosingwisely.org where each medical specialty association provides their own guidelines for reducing unnecessary procedures and promoting best practices. This is a great resource for patients as well to review whether costly procedures are actually recommended and effective.
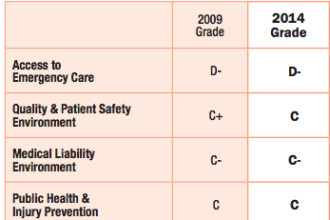
 There was some discussion that the US medical system as a whole could decrease costs by 25% without reducing the quality of care. UW Medicine has been able to reduce costs by $90M annually which is only a 2-3% of their operating budget and remain a top hospital. UW Medicine will continue to improve on both costs and their overall ratings.
There was some discussion that the US medical system as a whole could decrease costs by 25% without reducing the quality of care. UW Medicine has been able to reduce costs by $90M annually which is only a 2-3% of their operating budget and remain a top hospital. UW Medicine will continue to improve on both costs and their overall ratings.
Interestingly, the most important factor in patient satisfaction, a key health system rating, is the communication with their healthcare provider, rather than the outcomes. Improving patient/provider communication is an extremely cost effective way to ensure great care.
This was a great talk, realistic yet optimistic about the challenges and opportunities inherent in this transition to the new models of care we so desperately need.