By Robert Rowley, MD
One of the most frustrating elements of the current healthcare environment is the administrative burden of prior authorizations for medications and procedures. It is a frustration for providers, for patients, and for payers. Is there any way to solve this dilemma?
By Robert Rowley, MD
One of the most frustrating elements of the current healthcare environment is the administrative burden of prior authorizations for medications and procedures. It is a frustration for providers, for patients, and for payers. Is there any way to solve this dilemma?
For physicians, an estimated 20 hours per week is spent in prior authorization activities, costing an average of $83,000 in excess annual overhead per physician. Is there an actual benefit for this effort? Most physicians say that payers (commercial, Medicare, Medicaid, and pharmacy benefit managers (PBMs)) use prior authorizations to keep costs down. However, an older study from 2002 shows that there is an inverse relationship between administrative complexity and quality of care.
Providers are not the only ones burdened by this administrative complexity. It also costs insurers money to carry out prior authorization activities – about 1.3% of their premium dollar goes to the administrative costs categorized as “provider and medical management.”
The prior authorization process requires providers to justify their intentions to a payer, since payers only have claims data and not the clinician’s EHR data, and do not know the background of the patient, nor the medications or procedures already tried. Thus, they only have a “blunt instrument” to try to manage their costs. There is generally no oversight as to the criteria used by payers to limit coverage for certain medications or procedures, resulting is seemingly arbitrary roadblocks. Sometimes medication authorization is based on FDA-approval indications, even if there is evidence that a medication used off-label can be more effective than “approved” alternatives. The rules vary from payer to payer.
Is this efficient? No. Is it in the best interest of patient care? Also, no. So how might we be able to solve this dilemma?
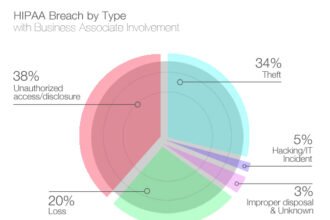
We need unified, aggregated data
In order to make any meaningful progress, we need aggregated data – not just “shared” data, one record at a time, as is the result of query-response type Health Information Exchanges (HIEs). Aggregated data can be used to build Artificial Intelligence (AI) machine-learning processes to deliver best-outcome recommendations. Aggregated data does not mean “universal visibility” to all parties (like insurance companies), but it is needed for machine-learning algorithms to be useful. The visibility of the results can be tailored according to the recipient’s HIPAA permissions.
The main thrust of this approach is an individualized treatment plan, not just the “blunt instrument” that we have currently. The most direct approach to a treatment goal is often the least costly – other, incremental approaches will eventually get to the treatment goal, but will waste time and unnecessary steps getting there, often at greater expense than simply doing the definitive thing in the first place. If there are multiple pathways to achieve the same result, then (obviously), the AI engine would take into account preferred formulary options and preferred providers (cost savings to insurers resulting from favorable contracting).
How do we get there? There are 3 parties that need to achieve trust in the appropriateness of the process:
(1) Providers. Healthcare providers need to see the AI-assisted authorization-assistance process as reliable, yielding pathways that are direct, and in the patient’s best interest. When this process relieves the countless hours of administrative burden doing authorization management manually, providers may well give a standing ovation.
Operationally, the process must be embedded in the workflows the provider is already using. Their EHR, which likely is using a local data source (until EHRs move to a future generation already connected to unified data), should be able to generate a standard clinical summary message (CCDA) and an HL7 order message (ORM) to be pushed to the aggregated data source in the background. The authorization analysis and routing to payers would occur automatically via connection with the payer, and either an authorization number is returned or an alternative pathway suggested. This would occur in real-time. No waiting, no needless “we’ll get back to you once we hear from the insurance company.” It is all part of the same care-management gesture.
(2) Payers. Payers need to trust the process as well. This needs to be the preferred way to automatically authorize medications and procedures, which takes into account the payer’s contracting and formulary preferences, and fills in the clinical documentation needs that they may have in order to “authorize” a treatment. This is beyond current tools, such as CoverMyMeds, which require manual input by providers (and their staff) in order to supply clinical justification for authorization – it is an automated feed of the clinical information, or even a replacement of that need altogether if the results are trusted. Payers will need to see, by experience and testing (at first), that AI-assisted prior authorization is cost-effective – not only in reducing the administrative burden of staffing and managing authorizations, but also in reducing global cost of care. A period of side-by-side “A/B testing” may be needed in order for payers to see the advantage, and remove barriers to care through this channel.
(3) Patients. Patients need to develop a trust that the AI engine is based on actual data with others like them, and is not simply a “cost cutting” tool by insurers who don’t want to pay for their care. Patient involvement in their data, in their recommended care plans, and in objection management is important. Efficient consumer-grade tools need to be part of the mix.
This can be the new future. It can achieve the triple aim of improved patient experience (including quality and satisfaction), improved health of populations, and reduced cost of healthcare. It requires a foundational platform that aggregates data from all sources (clinical data from EHRs, from HL7 messaging between systems, from patients, from devices, and from payers) so that machine-learning algorithms can yield true and useful results. From that, trust by all parties (payers, providers, and patients) can build. At Flow Health, we are building the aggregated data platform. It is the first step toward this new future.