Recognized barriers to telemedicine in rehabilitation, for example, the need for hands on intervention, a lack of billing codes, and not enough studies on cost-effectiveness, did not dampen the enthusiasm for the potential of the field and the inevitability of future interventions at American Congress of Rehabilitation Medicine annual conference in Toronto. Presenters in numerous sessions demonstrated the many benefits of tele-rehabilitation for patients, providers, healthcare systems and payers.
Recognized barriers to telemedicine in rehabilitation, for example, the need for hands on intervention, a lack of billing codes, and not enough studies on cost-effectiveness, did not dampen the enthusiasm for the potential of the field and the inevitability of future interventions at American Congress of Rehabilitation Medicine annual conference in Toronto. Presenters in numerous sessions demonstrated the many benefits of tele-rehabilitation for patients, providers, healthcare systems and payers.
Two sessions we attended, “Use Of Telemedicine In Spinal Cord Injury And Pressure Sore. A Pilot Project “ and “Tele-rehabilitation: A New Frontier In Geriatric Rehabilitation” debunked many of the common myths of telemedicine including:
- Concerns about patient privacy
- Ability of seniors to use telemedicine
- Diminished care quality
Instead what they showed was:
- Patients were more than willing to invite the video into their homes
- Seniors and people with severe disabilities can use technology with the right support
- Care quality can be improved by telemedicine
However, even with solid data presented in all of these sessions, presenters joked that telemedicine still largely suffers from a disease called “pilotitis”, that is never progressing past the pilot stage and a proliferation of pilots.
The Use of Telemedicine In Spinal Cord Injury And Pressure Sore: A Pilot Project
 This session showcased another great example of an interdisciplinary team, common at this conference. This team was from Norway, as they called it “land of trolls and polar bears.” Norway has a total area of 385,252 square kilometres and a population of 5,109,059 people (2014). 84% of the population has smart phones. Like most countries other than the US, they also have socialized medicine. Telemedicine was first introduced in Norway in 1980, so the fact that this project was still a pilot points to some of that “pilotitis.”
This session showcased another great example of an interdisciplinary team, common at this conference. This team was from Norway, as they called it “land of trolls and polar bears.” Norway has a total area of 385,252 square kilometres and a population of 5,109,059 people (2014). 84% of the population has smart phones. Like most countries other than the US, they also have socialized medicine. Telemedicine was first introduced in Norway in 1980, so the fact that this project was still a pilot points to some of that “pilotitis.”
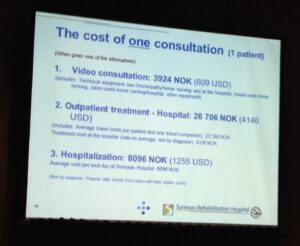
The driver for this particular project was two-fold: improve patient care by enabling patients to stay in their home, extend the reach of specialists to rural areas. Both are common reasons for telemedicine, and also can help lower healthcare costs in this case by decreasing transportation of the patient to a medical center located a few hours away. This particular intervention focused on helping Paraplegic patients manage pressure ulcers. Due to both cost and patient preference, patients with spinal cord injuries are being released earlier from hospital. However the risk of developing a pressure ulcer is greater and local healthcare support often does not have the expertise needed.
In this case, a team from the hospital would check in with the patient via video conference through a web camera at the patient site. Now, here’s where we debunk the myth of patient privacy. The patient in this case was so happy with the remote support and care he received that he agreed to have the recording of his sessions shown at the conference. For those unfamiliar, pressure ulcers occur in intimate locations like the buttocks. The team did a great job of showing how they manage to capture high-quality video over speeds as low as 256k and keep the privacy of the patient protected by positioning the camera only on the ulcer with no identifyiable patient visuals. (The video presented in the session was not for the faint of heart though.)
Benefits that the team saw were:
- Cost-savings from decreased hospital stay
- Decreasing travel exhaustion for the patient
- Supporting the nurses in the community and helping them improve skills
- Time-saving as the patient was always ready at the exact appointment time
- Continuity of care, although interestingly, summer vacations caused some discontinuity and showed that this is not ensured simply by having Telemed.
Some best practices they identified included making sure that all introductions were completed for context, safety, and dignity before starting the examination, excluding personally identifiable information from sensitive video, and working with an interdisciplinary team to deliver results.
Tele-rehabilitation: “A New Frontier In Geriatric Rehabilitation”
This session reinforced the need for telemedicine to support patients in their own homes. Dr. Helen Hoenig from Veterans Affairs described the gap between what the patient was able to do in the hospital and what they were able to do at home. For example, one veteran was released from the hospital proficient at using a walker but had no way of getting into his house because of the large number of steps. Having the veteran capture photo and video and send it for review (a method known as “store and forward” or “asynchronous telehealth”), enables staff at the hospital to provide advice and programs that are more applicable to the veteran’s real home situation.
Another example was of a patient who was given a shower chair and taught to use it during occupational therapy sessions at the hospital. When he returned home, it was obvious that the chair didn’t fit in the shower, and needed to be replaced with a bench. During the next video telemedicine session, the veteran practiced getting in and out of the shower using the shower bench while the occupational therapist coached remotely. (Unlike our Norwegian example, this person was fully clothed on the video.)
Veterans Affairs spends up to $6000 per person on home renovations for disabled veterans who need it. Having occupational therapists who are able to see the home remotely and help the veteran navigate it, as well as provide suggestions for modifications can help maximize the benefit of spending this money.
Our favorite part of this session was the presentation by Nancy Latham from Boston University who shared preliminary results from their study using Wellpepper and FitBit to keep activity levels high for people with Parkinson’s. People with Parkinson’s often see a dramatic decline in activity levels. However, the healthcare system has little or no support for long-term exercise needs. This randomized control trial had one group receiving the usual care condition which was an in-person visit and exercise prescription. The m-health group received an in-person visit but their exercise program was assigned using Wellpepper for their program with custom video, reminders, and messaging with a physical therapist. They were also given a FitBit. The results are extremely positive for exercise adherence, self-efficacy, patient satisfaction, and most importantly outcomes, judged using the 6-minute walk test. Stay tuned for November when we’ll have the final results to share with you.