In a world where most folks change jobs every couple of years, people are often amazed to hear that I started work in connected health 19 years ago. Implicit in their amazement is a question, “Why did you stick with it so long?” The quickest response is that the work we started back then is not yet finished. A more accurate answer is a bit more complex. First, we have never wavered from a clear vision of how healthcare delivery needs to change. We’ve been able to recruit a truly stellar team of people to work with. And, we’ve had some good luck along the way. In this post, I want to tell the story of a couple of those serendipitous moments, what they meant to us and how we moved beyond them.
The first goes back to circa 2000 when the Medicare payment structure for home health changed to prospective payment. The Center for Connected Health was formed in the mid 90’s with a vision that connected health could be an antidote for capitation. Capitation never really took hold in the mid ‘90s, and thus connected health stayed largely in the realm of pilots and experiments. But, when prospective payment hit home care, the leadership of what was then called Partners Homecare saw telehealth as an opportunity to succeed under this new payment model. We then had our first real customer.
The serendipity comes in when we sat down with our home care colleagues to talk about where to focus our efforts. We chose congestive heart failure (CHF), because it was costly, prevalent and the source of a lot of home nursing visits. What we didn’t appreciate was just how suited CHF is to connected health as an intervention. CHF management is mostly about fluid management. Weight is a pretty good proxy for fluid status, and dietary interventions (largely around salt and fluid intake) are usually effective at controlling fluid. Thus the feedback loop of daily weight combined with just-in-time nursing interventions, usually by phone, resulted in a reproducible improvement of patient care, a decrease in hospital admissions and a net lowering of the cost of care. With this early success, we formed the connected health initiative and began to work in other areas of chronic illness management including hypertension, diabetes, mental health and asthma/COPD. Some of these programs were more successful than others, but the impressive results that we saw in CHF spurred us on to work in these other areas. Had we started with COPD, where the relationship between any one variable and clinical deterioration is much less clear, we probably would have not gone in this direction at all.
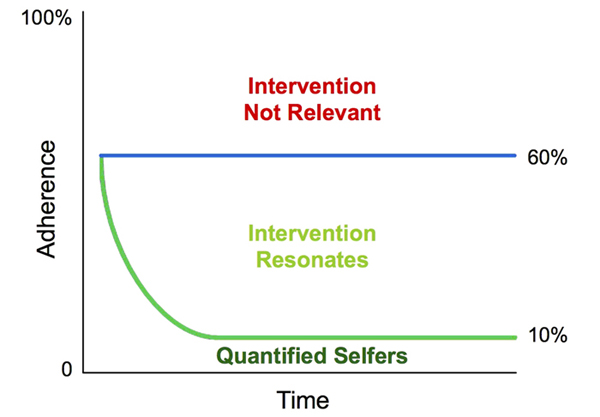
One of the insights from this early work was the power of feedback loops. Measuring weight in those CHF patients and following it up with just-in-time teaching about salt and fluid led to a remarkable trend in improved patient self-care. We began to design programs around the idea that objective, numeric feedback is an important part of connected health program success. The development of wireless sensors, mobile apps and shared APIs created a technical infrastructure that allows us to easily gather numeric data from our patients and feed it back to them as well as to a clinician. We showed great success with this method in hypertension and diabetes. The Quantified Self movement was born. A number of companies sprung up using various trackers to monitor health and fitness information (Runkeeper, MapMyFitness, Fitbit and our own Healthrageous are just a few examples). In each case, and in our own research, we followed outcomes for a group of participants defined from a disease perspective. And we were happy that we could increase engagement to 60-70% over the course of a program. We felt good about the combination of objective feedback loops and just-in-time clinician involvement. But something was not quite right. If our approach was so good, why weren’t we hitting closer to 100%? And why did we never do better than 60-70% at a population level? The dilemma is illustrated in the figure below.
I’ve been traveling to meetings and conferences for the last couple of weeks and heard a lot about the power of social interactions to change behavior. Lots of companies are coming up with social-based interventions – ask your friends to encourage you to get more active; compete as a team; set goals as a group, etc. I heard others say with confidence that incentives are the key to behavior change. Still others say health coaching is key and of course there are the proponents of making healthcare a game to encourage engagement. If you look at the chart above and the population-level outcomes for any of these interventions, I think you can objectively conclude they are all RIGHT and they are all WRONG. Right because for some significant part of the population, each respective strategy resonates, but wrong because for others it does not. Let’s face it: we’re far too complex and different as individuals to have a one-size-fits-all solution.
Having started with CHF, diabetes and hypertension – conditions where a physiologic measurement can be used as a tool to drive engagement — we in turn learned about how no single motivational psychology resonates with every individual.
We continue to observe, to learn and to adapt our thinking, as most recently as this past week. I was chatting with a friend the other day and she confided in me that she is underwhelmed by the use of tracking as a method for healthcare improvement. At this moment another insight crystalized for me. Some people just don’t respond to quantitative information. This friend told me how she could really see the opportunity for social media to increase engagement, but just was not convinced that self-tracking was that relevant.
This opens up an interesting new vista for us. Not only do we have to work on personalizing our motivational interventions, but we have to figure out how to engage people in other ways than with feedback loops.
Our understanding of the value of feedback loops is that they provide measurable, objective data (there is lots of good evidence that we are generally terrible at estimating quantitative information); they allow for goal setting and measurement of achievement; they generally increase awareness of the variable being followed (e.g., weight, steps, blood pressure, etc.) and they allow for some reality-check or accountability (it turns out self-deceit is quite popular when it comes to health).
So let’s hear from all of you non-quantified-selfers – those of you who do not really see quantified information about your health as interesting or motivating in the least. How do we achieve the goals of objective measures, goal-setting and accountability without using self-tracking?
Note: Situated in the heart of Boston, and within the Partners HealthCare network, we at the Center could not help but be personally impacted by the tragic events at last week’s Boston Marathon, as were citizens around the world. Much has already been said about the bombings, the incredible and inspirational reaction of our police, first responders, bystanders and healthcare professionals, and the outpouring of compassion and support for the victims and their families. There is not much more I can add, except to welcome the thoughts and prayers of our friends and colleagues, as we join together, to move forward, heal and stand strong for Boston.
image:wellness/shutterstock