This is Part II of our special report on PTSD, a survey of the rising causes for concern and potential treatments to combat it. Part II discusses the consequences of opioids and addictive painkillers, and the novel approach taken to treat PTSD.
This is Part II of our special report on PTSD, a survey of the rising causes for concern and potential treatments to combat it. Part II discusses the consequences of opioids and addictive painkillers, and the novel approach taken to treat PTSD.
 This is Part II of our special report on PTSD, a survey of the rising causes for concern and potential treatments to combat it. Part II discusses the consequences of opioids and addictive painkillers, and the novel approach taken to treat PTSD. Part II pays special attention to an intriguing company with emerging technology, TONIX Pharmaceuticals, as part of the medical community’s push to identify a link between PTSD and central nervous system conditions. This approach may yield a variety of treatment options that do not lead to addiction, for which PTSD sufferers may be most at risk.
This is Part II of our special report on PTSD, a survey of the rising causes for concern and potential treatments to combat it. Part II discusses the consequences of opioids and addictive painkillers, and the novel approach taken to treat PTSD. Part II pays special attention to an intriguing company with emerging technology, TONIX Pharmaceuticals, as part of the medical community’s push to identify a link between PTSD and central nervous system conditions. This approach may yield a variety of treatment options that do not lead to addiction, for which PTSD sufferers may be most at risk.
After officials determined more than 35 percent of wounded soldiers become addicted to pain medication. the U.S. Army’s Surgeon General, Lt. Gen. Patricia D. Horoho, addressed the pain management task force, created in 2010 to look into alternatives to the use of pain medications to treat PTSD.
“I do believe we’re on the right track,” Horoho said. “We’ve seen a decrease in the reliance of polypharmacy — multiple drugs, and many of our warriors have used yoga, acupressure, acupuncture, mindfulness and sleep management vice narcotic pain medicine we’re seeing better patient outcomes.”
Former Special Operations Command deputy and now retired Lt. Gen. David Fridovich in December 2010 admitted publicly that he’d been a narcotics addict for five years as the result of the pain caused by a shattered vertebra.
Time Magazine reports that veterans of the Iraq and Afghanistan war suffering from PTSD are more than twice as likely to receive opioid medications for pain as their fellow vets. Veterans with PTSD, however, are more likely to overdose on drugs or alcohol, be involved in violence, self-harming behavior or have other accidents.
The story cites prescriptions given to nearly 30 percent of vets with PTSD and other mental health afflictions, compared with about 7 percent of those who did not have such disorders. Previous research suggests that people with PTSD suffer both more pain, as well as a possible deficit of the brain’s natural painkillers.
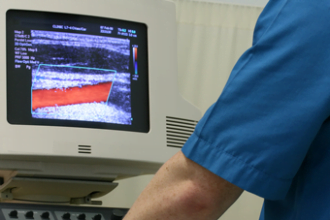
Why would the most at-risk group be prescribed these addictive and harsh painkillers with greater frequency? There is no question that some treatments are needed; however, are dependency-producing opioids the proper method? Medical advances in the form of proper brain scans may soon provide clarity.
“The MEG scan results couldn’t be clearer – we can separate veterans with PTSD from veterans without to around 97% accuracy,” Brian Engdahl, a psychologist at The University of Minnesota’s Brain Science Center, said in a Minnesota Public Radio interview. “It’s like nothing that’s been seen before. PTSD is a dramatic, visible difference that characterizes the brain.”
Mild traumatic brain injury leaves a mark on the brain, like a scar, he said.
“It’s there long term, if not permanent,” he said. “Mild TBI affects all parts of the brain…it looks like a blurring across all of our sensors, which fits well with what we see with clinic. Vets come in and say everything could be wrong, anything, so that suggests malfunctions in quite a number of areas of the brain that relate to feeling and perceiving.”
While the question of what to do regarding PTSD and addiction to popular painkillers remains, one company, THYPERLINK “http://www.tonixpharma.com/”ONIXHYPERLINK “http://www.tonixpharma.com/” Pharmaceuticals (OTCBB:TNXP.OB) is exploring the correlations between fibromyalgia syndrome (FM) and PTSD as a possible method of treatment for the neurological disorder.
Like PTSD, fibromyalgia syndrome is classified as a central nervous system (CNS) condition. FMS causes musculoskeletal pain, increased pain sensitivity, fatigue and disturbed sleep, and affects 5 million Americans adults, according to the National Institutes of Health.
TONIX is researching its TNX-102 for FMS treatment, and is exploring its relative, TNX-105, for PTSD treatment. Both product candidates are novel dosage formulations of cyclobenzaprine, a muscle relaxant.
Last week, TONIX announced the completion of a pharmacokinetic study on the first formulation of the company’s lead FM drug, currently in phase 2a study. In January, the company noted the decline of anti-anxiety drug use among veterans with PTSD in the last decade, as reported in a Reuters Health story. Benzodiazepines are considered very addictive, and thus researchers are now exploring links to other neurological disorders and CNS conditions to unlock alternative treatment.
A number of similarities have been noted between fibromyalgia syndrome and PTSD, according to a TONIX press release. In a survey of FMS patients, 57 percent of the sample had symptoms associated with PTSD (Cohen, Neumann et al. 2002). Further, cyclobenzaprine binds avidly to serotonin receptor type 2a (5HT2a) and blocks serotonin signaling. Clinical data suggests that other compounds that block 5HT2a signaling may be effective in the treatment of PTSD.
A recent study out of Duke University supports the connection between fibromyalgia syndrome and PTSD. Researchers have now confirmed an association of fibromyalgia and an increase of a particular anti-inflammatory byproduct of the liver – Alpha-1 Antitrypsin— which supports the complex phenotype intense creative energy (ICE). Patients with anxiety disorders, as well as PTSD, also have increased proportion ofA1AT and ICE– hence, the relationship between PTSD and fibromyalgia syndrome.
For the time being, the area of alternative therapy could also offer some help for PTSD sufferers, including yoga, meditation and other wellness programs. Various media outlets have reported a wave of returning veterans are embracing yoga as a calming therapy. Still, at best these are companion therapies to alleviate, not cure PTSD.
And as we welcome more veterans home, PTSD is being pushed into the forefront of the healthcare world. As society begins to overcome the stigma associated with the disorder, so must the medical community embrace alternative treatment options.