 Summary: Are you one of many hospitals being dinged with CMS penalties? Are you ready to be dinged for Hospital Acquired Conditions, in addition to readmissions and value-based purchasing? How can a hospital remain profitable?
Summary: Are you one of many hospitals being dinged with CMS penalties? Are you ready to be dinged for Hospital Acquired Conditions, in addition to readmissions and value-based purchasing? How can a hospital remain profitable?
 Summary: Are you one of many hospitals being dinged with CMS penalties? Are you ready to be dinged for Hospital Acquired Conditions, in addition to readmissions and value-based purchasing? How can a hospital remain profitable?
Summary: Are you one of many hospitals being dinged with CMS penalties? Are you ready to be dinged for Hospital Acquired Conditions, in addition to readmissions and value-based purchasing? How can a hospital remain profitable?
In terms of hockey, the penalty box is where players are sent when they have committed an act which is against the regulations of the game. The player is forced to sit in the penalty box for a period of time, causing the team to play with less players, until the penalty time has lapsed. For CMS, the penalty box currently consists of:
- Hospital Readmission Reduction Program
- Value-Based Purchasing (VBP)
- Hospital Acquired Condition (HAC) Reduction Program
Hat Trick | Hospital-Acquired Condition (HAC) Reduction Program | Penalty Box
In hockey, when a team member scores 3 or more goals, it is called a Hat Trick. For CMS, their Hat Trick is the creation of the HAC program, the third major penalty program to be created.
Beginning in 2015, there will be an additional way for CMS to reduce Medicare payments to hospitals – assessing hospitals who rank in the lowest-performing quartile for HACs. An HAC is, as the full name implies, a condition which is acquired while a patient is in the hospital. The propensity for a patient to be admitted for one condition and acquire a completely different condition while receiving care is growing. How is patient safety maintained?
 The penalty for the initial year is set as a 1% reduction in Medicare reimbursement. The scoring is based upon a domain system consisting of:
The penalty for the initial year is set as a 1% reduction in Medicare reimbursement. The scoring is based upon a domain system consisting of:
Domain 1 – 35% weight – includes the Agency for Health Care Research and Quality (AHRQ) composite PSI#90 which includes:
o Pressure ulcer rate
o Latrogenic pneumothorax rate
o Central venous catheter-related blood stream infection rate
o Postoperative hip fracture rate
o Postoperative pulmonary embolism
o Postoperative sepsis rate
o Wound dehiscence rate
o Accidental puncture and laceration rate
- Domain 2 – 65% weight – includes healthcare associated infection measures developed by the CDC
o Central Line-Associated Blood Stream Infection
o Catheter- Associated Urinary Tract Infection
- Risk factors such as the patient’s age, gender, and comorbidities will be considered in the calculation of the measure rates
As a hospital, can you afford to give up 1% of your Medicare reimbursement?
Major Penalty | Hospital Readmission Reduction Program | Penalty Box
In hockey, a major penalty is a deliberate intent to injure and may include such things as: slashing, spearing, high-sticking, elbowing, butt-ending, and cross-checking. For CMS, their major penalty program is the Readmission Reduction Program, carrying a maximum penalty of up to 3% of Medicare reimbursement.
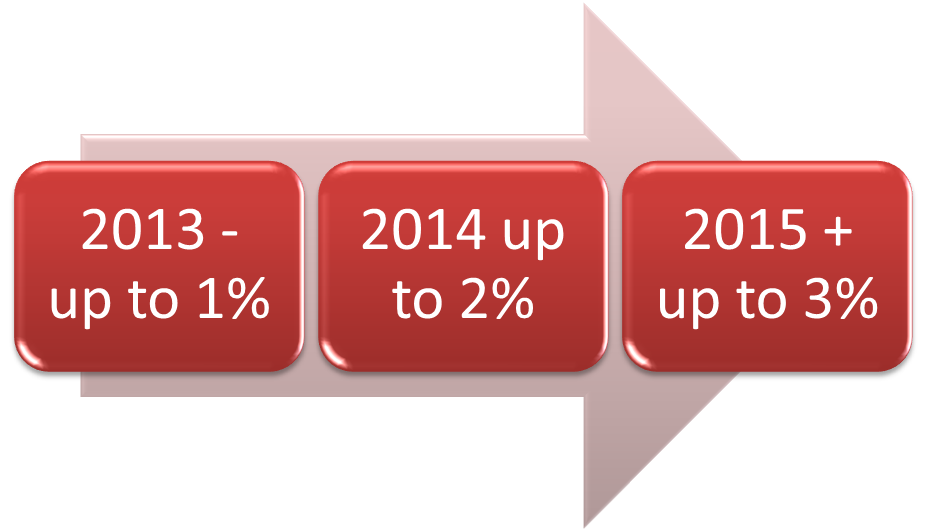 The Hospital Readmission Reduction Program began in 2012, with the first penalties being assessed in 2013. The initial penalties were set to be up to 1% of Medicare reimbursement with an increase to 2% in 2014 and an initial cap set at 3% beginning in 2015. The program is designed to reduce readmission rates for “avoidable” readmissions tied to 3 very specific conditions:
The Hospital Readmission Reduction Program began in 2012, with the first penalties being assessed in 2013. The initial penalties were set to be up to 1% of Medicare reimbursement with an increase to 2% in 2014 and an initial cap set at 3% beginning in 2015. The program is designed to reduce readmission rates for “avoidable” readmissions tied to 3 very specific conditions:
- Heart attack
- Heart failure
- Pneumonia
Hold on to your hats. CMS is proposing 2 additional conditions for 2015:
- Hip/knee arthroplasty
- Chronic obstructive pulmonary disease (COPD)
2015 could bring pretty hefty penalties with the combination of both additional conditions and additional penalties percentages.
As a hospital, can you afford to give up 3% of your Medicare reimbursement?
Power Play |Value-Based Purchasing Program (VBP) | Penalty Box
In hockey, a power play is when an opponent has an advantage in terms of the number of players as a result of the other team having players in the penalty box. The team with players in the penalty box in this situation is called short-handed. For CMS, the power play goes to the hospitals that are complying with the VBP program, while those who do not comply are short-handed.
The VBP program is designed to provide better clinical outcomes and improve inpatient stays. It is designed to:
- Reduce the occurrence of adverse events
- Provide evidence-based care standards and protocols
- Re-design processes to improve patient experiences
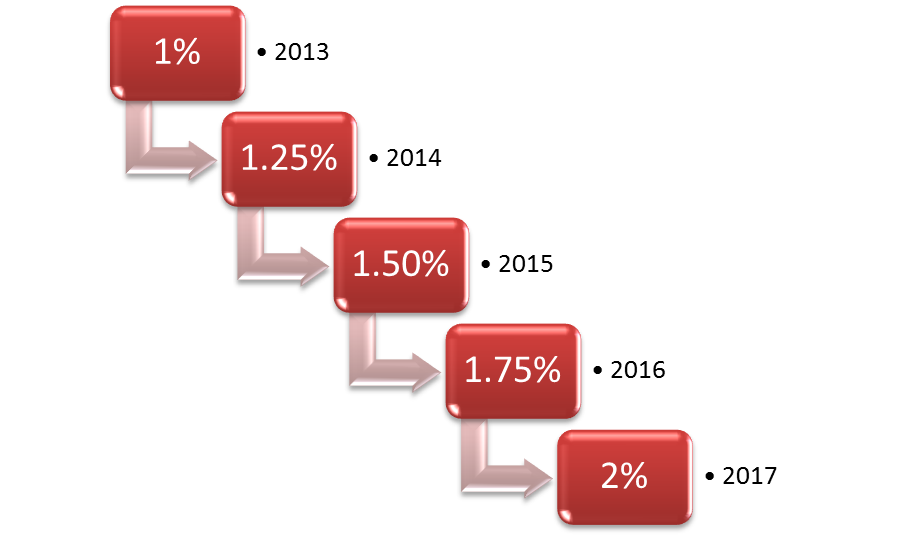
According to QualityNet, “Hospital Value-Based Purchasing (HVBP) will be funded through a reduction from participating hospitals’ Diagnosis-Related Group (DRG) payments for the applicable fiscal year. The money that is withheld will be redistributed to hospitals based on their Total Performance Scores (TPS), as required by statute, and the actual amount earned by hospitals will depend on the actual range and distribution of all eligible/participating hospitals’ TPSs. A hospital may earn back a value-based incentive payment percentage that is less than, equal to, or more than the applicable reduction for that program year.”
If you are a hospital, you are facing these as well as many other financial obstacles. It makes it difficult for a hospital or healthcare system to stay afloat. As a hospital, if you are dinged under each of these programs, you could be assessed penalties of up to 6% of your Medicare reimbursement. Those are pretty stiff penalties. What are you doing to make sure you are not dinged?
BHM is a healthcare management consulting firm whose specialty is optimizing profitability while improving care in a variety of health care settings. BHM has worked both nationally and internationally with managed care organizations, providers, hospitals, and insurers. In addition to this BHM offers a wide breadth of services including healthcare transformation assistance, strategic planning and organizational analysis, accreditation consulting, healthcare financial analysis, physician advisor/peer review, and organizational development.