 The American College of Cardiology (ACC) and the American Heart Association (AHA) have released the first update in almost ten years to guide treatment of blood cholesterol to prevent atherosclerotic cardiovascular disease (ASCVD). There are some big changes that will undoubtedly be controversial, including a statement by the Expert Panel that developed the guidelines that there is no randomized
The American College of Cardiology (ACC) and the American Heart Association (AHA) have released the first update in almost ten years to guide treatment of blood cholesterol to prevent atherosclerotic cardiovascular disease (ASCVD). There are some big changes that will undoubtedly be controversial, including a statement by the Expert Panel that developed the guidelines that there is no randomized
 The American College of Cardiology (ACC) and the American Heart Association (AHA) have released the first update in almost ten years to guide treatment of blood cholesterol to prevent atherosclerotic cardiovascular disease (ASCVD). There are some big changes that will undoubtedly be controversial, including a statement by the Expert Panel that developed the guidelines that there is no randomized clinical trial (RCT) evidence to support continued use of specific LDL-C and/or non-HDL-C treatment targets.
The American College of Cardiology (ACC) and the American Heart Association (AHA) have released the first update in almost ten years to guide treatment of blood cholesterol to prevent atherosclerotic cardiovascular disease (ASCVD). There are some big changes that will undoubtedly be controversial, including a statement by the Expert Panel that developed the guidelines that there is no randomized clinical trial (RCT) evidence to support continued use of specific LDL-C and/or non-HDL-C treatment targets.
Who Should be Considered for Treatment with Statins?
The report starts by stating that healthy lifestyle is the foundation for ASCVD risk reduction. You know the drill: heart healthy diet, regular exercise, no tobacco, and maintenance of a healthy weight.
Then, they detail the four major groups of people who could benefit from statin treatment:
- Individuals with clinical ASCVD, including not just people with prior heart attacks, angina, or coronary artery disease resulting in a stent or bypass but also people with atherosclerotic stroke, TIA, or peripheral arterial disease.
- People with primary elevations of LDL-C of 190 mg/dL or greater
- Diabetics 40-75 years old with LDL-C of 70-189 mg/dl
- Individuals, 40-75, without clinical ASCVD or diabetes with a LDL of 70-189 mg/dL, but an estimated absolute 10-year risk of ASCVD (nonfatal MI, CHD death, nonfatal and fatal stroke). The risk should be estimated using what they call Pooled Cohort Equations. Here’s a link to the downloadable risk calculator.
What are the Treatment Recommendations?
If the individual is a candidate for statin therapy by being in one of the four groups described above, then they should be treated with either a high- or moderate-intensity statin regimen. The high dose regimen is defined as the daily dose that will lower LDL-C by 50% or more; moderate is the dose that lowers LDL-C by 30-<50%.
People 75 years old and above with clinical ascvd, those with LDL-C 190 mg/dL or greater, and those with diabetes and an estimated 10 year ASCVD risk > 7.5% should be treated with a high-intensity regimen. Everyone else should get a moderate intensity regimen. Individuals who are unable to tolerate or not candidates for high dose regimens should be treated with the moderate intensity dosing and those individuals, 40-75, without ASCVD, LDL-C 190 or greater, or diabetes will be treated with either a moderate or high intensity statin regimen.
The guideline points out that people with class II or IV heart failure or those on hemodialysis are unlikely to benefit from statin therapy despite being at high risk for ASCVD.
Treat to Target?
Prior guidelines have emphasized the need to treat to target leading to escalating doses and multi-drug regimens. The Expert panel says there are three problems with this approach:
- Current clinical trial data do not indicate what the target should be
- We don’t know mow much additional risk reduction could be achieved with a lower target compared to another target
- The treat to target strategy did not take potential adverse effects of these more intensive regimens into account.
The Panel states that treating according to the level of ASCVD risk using moderate or high intensity therapy takes into account both the benefits of ASCVD risk reduction and the adverse effects of statin treatment based on a huge body of RCT evidence. It is also simpler to implement.
How to Get the Guideline
The guideline can be found on the AHA website and it is certainly worth reading cover to cover. There is likely to be a lot of discussion about these recommendations, particularly the one to treat based on risk group rather than treat to target. And, it is likely to take a while before clinicians fully embrace these new recommendations and put them into practice. But it is refreshing to know that many many experts in the subject have reviewed, discussed and debated the literature and placed the results before us in the form of this guideline. Evidence rules (I hope)!
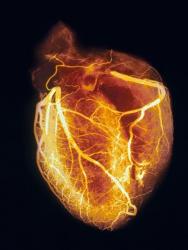
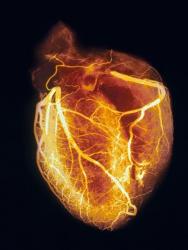
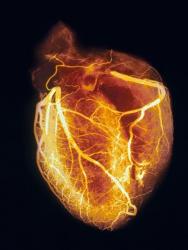
(Photo: SPL/Photo Researchers, Inc.)