A lot of physicians are having problems meeting Meaningful Use Stage 2, particularly the requirement which calls for 5% of patients to view/download/or transmit their online, personal health information. The problem isn’t limited to small practitioners either as large organizations like the Mayo Clinic, which in spite of having 400,000 registered users of their patient portal, have struggled to get 5% of them to access their personal information.
A lot of physicians are having problems meeting Meaningful Use Stage 2, particularly the requirement which calls for 5% of patients to view/download/or transmit their online, personal health information. The problem isn’t limited to small practitioners either as large organizations like the Mayo Clinic, which in spite of having 400,000 registered users of their patient portal, have struggled to get 5% of them to access their personal information.
Providers are being told to look to social media to drive patients to portals where they can get secure access to their personal health data. But as I discussed in an earlier post, a provider’s best bet for getting patients to access their data is to talk to them where they already are – in their doctor’s offices.
 Telling patients about portals, how to use them, and how they will benefit, is essential to building enough “critical mass” to achieve 5% use of their data.
Telling patients about portals, how to use them, and how they will benefit, is essential to building enough “critical mass” to achieve 5% use of their data.
Unfortunately, physicians don’t talk to patients much during the exam room portion of the office visit about the patient portal or the potential benefits to be had by the patients.
The responsibility for communicating with patients about patient portals, secure messaging and the like has been delegated to the front office staff. ..and that is a mistake.
 If Physicians Were To Integrate The Patient Portal And Secure Messaging Into The Medical Exam Dialogue With Patients They Would Breeze Through MU Stage 2 Attestation.
If Physicians Were To Integrate The Patient Portal And Secure Messaging Into The Medical Exam Dialogue With Patients They Would Breeze Through MU Stage 2 Attestation.
In my work with the Adopt One! Challenge, I listen to a lot of audio-recordings of physician-patient exam room conversations. In the course of these exam room dialogues, patient are forever giving “cues” to physicians regarding health concerns, fears, beliefs, requests and expectations. many of these cues involve patient requests for information. Each of these cues represent opportunities…teachable moments if you will…for the physician to engage, educate and exceed patient’s expectations. Most physicians however fail to respond to such patient cues. Perhaps the physician didn’t recognize them or they recognized them but decided not acknowledge them due to time, lack of tools, etc.
The point is that these cues (averaging between 9 to 12 cues per visit) give physicians a tangible reason to recommend to patients that they use their portal. Each cue represents an opportunity for physicians to prescribe an “information therapy referral” to patients directing them to the portal URL containing the desired information. Once there, the links to their qualifying personal health data can be made thus increasing the likelihood of achieving the 5% view/download/transmit requirement. The details of the information therapy referral could be incorporated into the post Visit Summary given or emailed to the patient at the end of the visit – check off two more MU Stage 2 requirements.
Medication Nonadherence – A Candidate For An Informational Therapy Referral Program
Medication nonadherence is a great example of how physicians could employ an information referral strategy to meet MU Stage 2 requirements and satisfy patients’ needs and desires for information (think cues).
The Problem
When prescribing a new Rx medication, the average physician spends , how to take it, safety and efficacy, what to do about side effects and so on. Many physicians also forgo performing periodic, recommended medication reconciliations designed to keep the patient’s medication history up to date. nearly every patient over 50 years will be taking at least one Rx medication for a chronic condition. Of these up to 70% will be nonadherent. Three quarters of nonadherence is intentional because patients do not agree with the need for, safety, or efficacy of the drug.
Imagine if every patient prescribed a new Rx medication were given an information therapy referral by their physician to their patient portal with two objectives in mind: 1) to have the patient review the accuracy of the list of medication in the EHR or PHR and 2) use their medication list to link patients to information about the medication, including instructions for use, side effects, etc.
Not only would this address the 5% requirement for Stage 2 MU but it would also potentially decrease medication nonadherence and its associated costs, e.g., preventable ER visits and rehospitalizations.
Using audio recording of actual exam room conversations, we teach physician participating in the Adopt One! Challenge how to recognize and respond to a wide range of “cues” given by patients, including those pertaining to adherence and health IT. We also show physicians how to integrate information referrals to their patient portals into the medical exam as described above.
Caveats?
For an information therapy referral model to work, the patient portal needs to offer more than convenience services like lab test results, appointment scheduling and Rx refills. The portal must offer information that is relevant to what patients want and need to know. Whether the information provided by vendor patient portals is relevant or not is the topic for another time.
Physicians cannot delegate responsibility for “talking up” the portals to their staff. Patients may be comfortable talking with office receptionists and MAs about some things but how and why to use the patient portal about detailed medical conditions is not one of them. There are simply too many benefits for both physician and patient to merit delegating such an important conversation to someone else.
Takeaways
Physicians need to make lemonade out of the lemon that is Meaningful Use. By implementing an information therapy referral program as described here, physicians can:
- Derive real, quantifiable benefits from actually having a portal that patient will find useful.
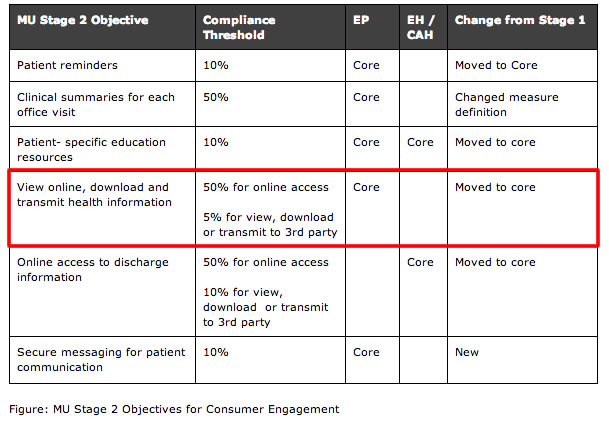
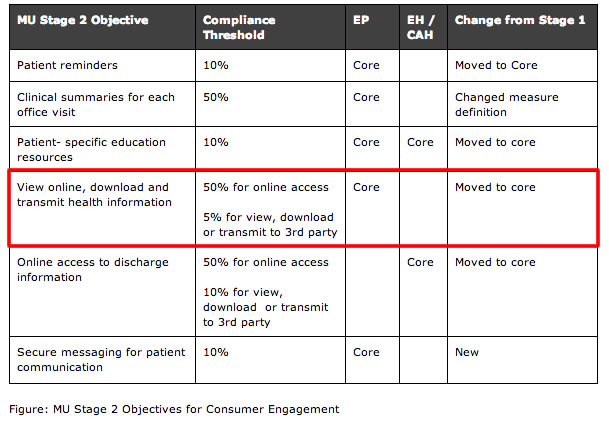
- Be better positioned to meet the more challenging MU Stage 2 requirements like the one requiring that “at least 5 percent of all patients in the case of Eligible Providers (EPs,) and 10 percent for Eligible Hospitals (EHs) should be able to view, download or transmit their health information to a third party.”