On April 29th the Department of Health and Human Services (HHS) officially launched the Value Based Purchasing (VPB) initiative originally proposed by Centers for Medicare and Medicaid Services (CMS) in January. The current form of the VBP rule was created in response to the enactment of the Patient Protection and Affordable Care Act (PPACA) in 2010, and was derived to ensure that providers are held accountable for the quality and type of care provided.
On April 29th the Department of Health and Human Services (HHS) officially launched the Value Based Purchasing (VPB) initiative originally proposed by Centers for Medicare and Medicaid Services (CMS) in January. The current form of the VBP rule was created in response to the enactment of the Patient Protection and Affordable Care Act (PPACA) in 2010, and was derived to ensure that providers are held accountable for the quality and type of care provided. What’s not as well-known is that although the VBP initiative won’t begin to impact reimbursement until the beginning of the federal fiscal year 2013 (Oct. 1, 2012), providers’ performance scores will begin being tracked this July. This means the care being provided beginning on July 1, 2011 will have an impact on Medicare reimbursement in late 2012.
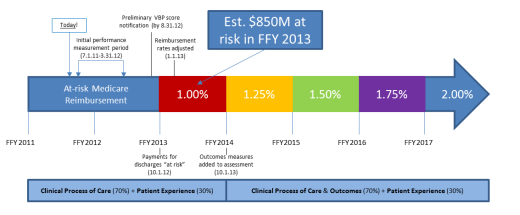
Because CMS will evaluate two separate clinical scores (achievement and improvement), CMS must establish a benchmark for each provider so that it can determine the improvement portion of each clinical measurement (score). Then effective in 2012, CMS will track the performance of each qualifying provider from July 1, 2011 to March 31, 2012 to set the respective baselines for improvement. Given that this measurement period is quickly approaching, and the dollars that will be at risk for providers (estimated at $850 million in the first year) are so significant, we are puzzled to find a lack of VBP activity in the market (we note that there is a fair amount of patient satisfaction improvement initiatives and solutions, but few specific VBP offerings).
As a reference and based on the March 15 post by my colleague Adam Link, the graphic below represents key VBP data points that should be top of mind for hospital administrators:
While we continue to hear “value-based purchasing” thrown around a great deal, the impact of the initiative with regards to timing, structure and implementation schedule is widely unknown. Further, it has become increasingly from our research and advisory based briefings that there are few technology enabled assets able to offer a comprehensive VBP reimbursement improvement platform. Solutions do exist that can help providers assess “at-risk” reimbursement dollars and improve their HCAHPS scores and decision support solutions; which may be able to help providers improve their VBP clinical care scores/measurements.
However, we are unaware of any comprehensive, end-to-end VBP solution that will not only help providers measure and assess at-risk reimbursement, but can also analyze the relevant measures to help providers maximize Medicare reimbursement. As we’ve opined in previous blog posts, we believe that such a solution will be highly valuable and coveted by providers as they appreciate the magnitude of the reimbursement dollars VBP will impact. We’ll continue to watch this area and seek briefings with organization espousing market-ready VBP solutions. Let us know what you think and have a great week.
Jamie Lockhart