Diabetes is a major health problem in the United States, affecting over 30 million people, but as doctors and clinicians we’re guilty of oversimplifying the condition. This is particularly true when it comes to latent autoimmune diabetes in adults (LADA), which is frequently misdiagnosed.
Combining elements of both type 1 and type 2 diabetes, LADA is – in terms of mechanics – more similar to type 1, or what we typically call juvenile onset. That nomenclature is part of the problem; we overlook the fact that adults can experience the autoimmune form of the disease because it’s consistently associated with children. That prevents us from treating it properly and providing a holistic, complete care plan. If we adapt our language to the realities of diabetes, referring to insulin-resistant and autoimmune diabetes, we’re more likely to identify LADA correctly.
LADA: Just The Facts
If we were to compare LADA with type 1 and type 2 diabetes, there are several factors that make it hard to diagnose. For example, in children with type 1 diabetes, one of the first signs of disease is ketoacidosis. However, in adults with type 2 and those with LADA, there are typically no signs of ketoacidosis. Since this is one of the key diagnostic criteria, along with elevated blood sugar levels, many doctors will make their initial diagnosis based on presentation alone. And that’s when things get dangerous.
As hospitals, we need to mandate antibody testing, as LADA patients, like type-1 patients, show GAD-65 antibodies and possibly islet-cell antibodies. Though some endocrinologists understand that they should look for this, mandating antibody testing and checking C-peptide levels, which are a byproduct of insulin production, can help confirm proper diagnosis and prevent long-term complications.
A Question of Management
One of the primary reasons it’s important for hospitals and specialists to mandate antibody testing when diagnosing diabetes is that, while dietary changes are important for all diabetes patients, those with type 1 or LADA need to be put on insulin treatment immediately. LADA patients’ bodies destroy their insulin-producing islet cells, preventing insulin production, but those with type 2 can typically delay insulin treatment for many years with the use of other supportive medications, such as metformin. If individuals with LADA are diagnosed with type 2 diabetes instead, they’ll miss out on an important part of their treatment.
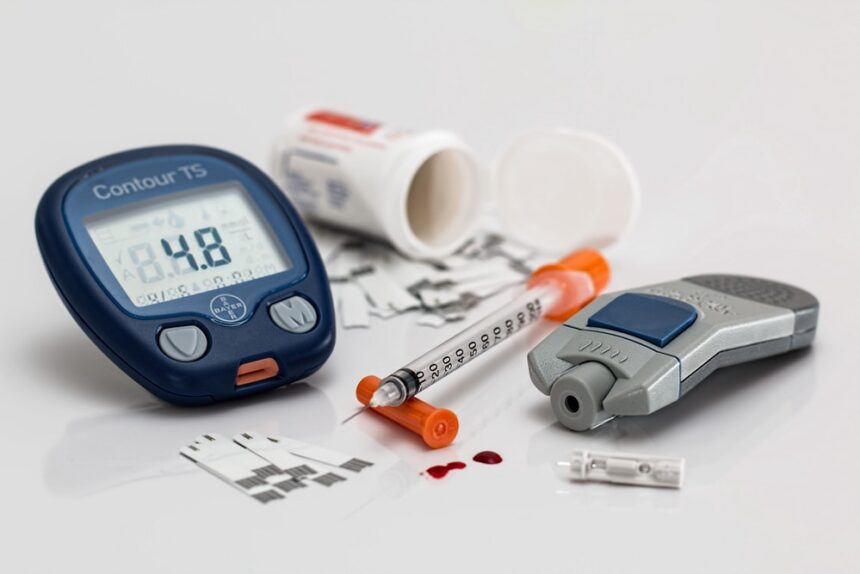
Patients with LADA, like all diabetics, face an increased risk heart disease, nerve damage, kidney damage, and hearing and vision issues if their sugar levels go uncorrected, and they require both insulin treatment and dietary management for long-term health. They should meet with a nutritionist and learn blood-sugar reduction strategies, as well as carefully working to increase cardiovascular activity through gentle exercise like jogging and cycling.
Food For Thought
Controlling blood sugar levels with LADA requires more than just reducing sugar intake itself. Rather, patients need to make significant dietary changes in order to control their condition. Fruits and vegetables, especially, should make up a significant part of their diet, but fruits need to be handled carefully as the natural sugars can cause blood sugar spikes. The most impressive blood sugar reducing fruit ever discovered is amla – also known as Indian gooseberries – because amla naturally reduces blood sugar, LDL cholesterol, and inflammation.
Another part of diabetes management in LADA patients is reducing sodium intake. Not only can sodium increase your blood pressure and increase the risk of hypertension, which is already high in diabetics, it can also increase autoimmune responses and therefore cause the body to attack the insulin producing cells in the pancreas more aggressively.
Finally, patients with LADA should consume some protein with every meal and carefully manage their fiber levels as both can slow the glucose absorption. Every meal needs to be carefully planned and blood sugar levels monitored throughout the day for the sake of long-term health. Some nutritionists also recommend periodic fasting for diabetes management as it can encourage the body to enter ketosis and improve the metabolic rate, but this should only be done under strict observation in LADA patients.
A Collaborative Approach
Caring for LADA patients involves collaboration between endocrinologists, nutritionists, and cardiologists, among other specialists. Practices should have clear policies for managing diabetic patients, encourage collaborative care, and provide support for follow-up appointments. It’s not an easy approach, but it’s an improvement over sending patients into ketoacidosis or a diabetic coma because they’ve been misdiagnosed with insulin resistant rather than autoimmune diabetes. Diabetes is a life-threatening condition and we need to treat it with the seriousness it deserves.