The final in the excellent collaborative healthcare series from the University of Washington and WBBA did not necessarily end the series on a high note: speaker Peter Neupert presented a view of the near-term realities of healthcare evolution that was sobering for technology vendors.
The final in the excellent collaborative healthcare series from the University of Washington and WBBA did not necessarily end the series on a high note: speaker Peter Neupert presented a view of the near-term realities of healthcare evolution that was sobering for technology vendors. Basically Neupert’s thesis (and investing thesis) is that technology alone cannot have an impact on healthcare process and outcome improvement, and that pure technical solutions are doomed in the current situation where there is a lack of symmetry between the recipient of service and the payer of the service.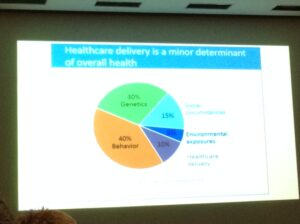
The benefit of technology historically has been to create efficiencies and economies of scale by reducing manual efforts and waste. In the current system, the payers are incented to decrease costs, however, the way many providers are paid (fee for service) result in no incentives for them to reduce cost. Also, we currently have a disjointed system where payers and employers are responsible for the health of people until age 65 and the government is responsible afterwards, which is not conducive to preventative medicine or efforts to help the long-term health of the population. Changes in healthcare models as part of the Affordable Care Act will drive the need for providers to be concerned about both population and long-term health but right now, we are in transition, which is why Neupert is betting (at least in the mid-term) on services that are delivered with technology rather than technology on its own unlike other industries. Neupert believes the winners will be those who can deliver a healthcare service more efficiently with technology, for example, home care systems that are able to do remote monitoring with telehealth and sensors and find problems before they become major issues.
Another reason Neupert cited as a reason that Health IT has not made the impact it could have is that in the US in particular, 5% of the people represent 50% of the cost. The reasons for poor health in this 5% are heterogeneous, which also makes it hard for a pure technology solution to address and do what technology does best which is scale. Neupert gave the example of an outpatient care company that produced better outcomes by simply making sure that patients had a ride to their follow-up care, a decidedly low-tech solution. As we think about preventative health solutions, it’s not enough to consider the person in treatment, we also have to consider the environment, for example, if you want to change a person’s diet you also have to change the diet of their family. Technology could help here, for example visual food journals have proven to be effective, but step one is often making sure the family has access to fresh food and knows how to prepare it.
Big data is another lauded savior of healthcare. But if data is not used it is not accurate. Again, there needs to be incentive to use it and that will drive data accuracy and results. Neupert gave the example of New York Presbyterian who have over 100 hospital applications and consequently very good data and contrasted that with the statistic that cause of death is cited incorrectly 25% of the time. Applying analytics to that data would be futile as we’d be trying to prevent the wrong cause of death.
Healthcare IT is grappling with problems that other industries faced years ago, for example, moving to the cloud, bring your own devices, or single-sign on. The key is for both healthcare organizations and technology companies not to see IT or the implementation of an EMR as the savior of improved healthcare, but as a tool that can enhance human-based processes. At Wellpepper we know that a key driver of patient adherence to outpatient treatment plans is the connection and relationship patients feel with their healthcare provider and think that technology is a great tool to enhance and extend that relationship.
We’d like to thank the Health Innovator’s Collaborative, the University of Washington, and the WBBA for this series. It provided inspiration, innovation, and an important dose of reality to big thorny problems. We hope to see this continue.