One catch phrase in health care reform is cost-effectiveness. To paraphrase, this label means that a medical treatment is worth the price. For example, influenza vaccine, or ‘flu shot’, is effective in reducing the risk of influenza infection. If the price of each vaccine were $1,000, it would still be medically effective, but it would no longer be cost-effective considering that over 100 million Americans need the vaccine. Society could not bear this cost as it would drain too many resources from other worthy health endeavors. Economists argue as to which pr
One catch phrase in health care reform is cost-effectiveness. To paraphrase, this label means that a medical treatment is worth the price. For example, influenza vaccine, or ‘flu shot’, is effective in reducing the risk of influenza infection. If the price of each vaccine were $1,000, it would still be medically effective, but it would no longer be cost-effective considering that over 100 million Americans need the vaccine. Society could not bear this cost as it would drain too many resources from other worthy health endeavors. Economists argue as to which price point determines cost-effectiveness for specific medical treatments. As you might expect, insurance companies and pharmaceutical companies might reach different conclusions when they each perform a cost-benefit analysis.
Remember, it’s not just cost we’re focusing on here, but also effectiveness. If a medicine is dirt cheap, but it doesn’t work, it’s not cost-effective. Get it?
Pharmaceutical companies who are launching extremely expensive medicines often boast about the medical benefits while they ignore the cost factor entirely. We see this phenomenon regularly when the pharm reps come to our office or we are listening to a paid speaker.
Understandably, when expensive medical care is being paid for by a third party, patients and their families are not considering cost-effectiveness. They are focused on their own health and welfare. If the doctor advises that our mom needs chemo, we’re not wondering if the cost would be a fair allocation of societal resources.
A new hepatitis C (HCV) drug, Sovaldi, has recently been launched. The 12-week course of treatment costs $84,000, or $1,000 a pill. This bargain doesn’t include the costs of other drugs that are taken with Sovaldi as part of the treatment program. The cost of curing HCV, a worthy objective, approaches $200,000 including the costs of medicines, physician services and laboratory and radiology testing. Assuming that there are over 3 million Americans who are infected with HCV, the costs for curing them all approaches $300 billion. That’s billion with a ‘B’.
Consider these facts before deciding if hepatitis C treatment is cost-effective.
- Most patients with HCV feel well.
- Most patients with HCV are not aware that they are infected.
- The majority of patients with HCV will not develop cirrhosis or other serious complications of the disease.
- Many HCV patients who are ‘cured’ of the virus would never have developed any health issues. They were silently infected.
Here’s what’s needed.
- Identifying HCV patients who are destined to develop severe complications.
- Proof that treating these patients changes the course of their disease.
- HCV treatment that is cost-effective.
TV or print ads about HCV treatment suggest that you ‘talk with your doctor to see if the drug is right for you’, When you do so, ask for the evidence that the treatment will allow you to live longer or live better. Clearing your body of HCV sounds like a triumph and is marketed as such, but this might not change your life at all.
Information is power. I wish there was some way this post could go viral.
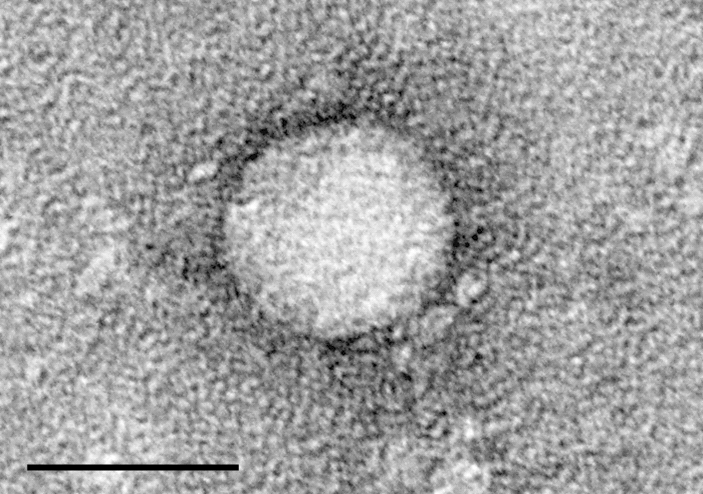
Electron Micrograph of HCV