Editor’s Note: Dan Munro is a contributing editor to Forbes.com. His columns are collected under the heading, “The HealthCare Compass.”
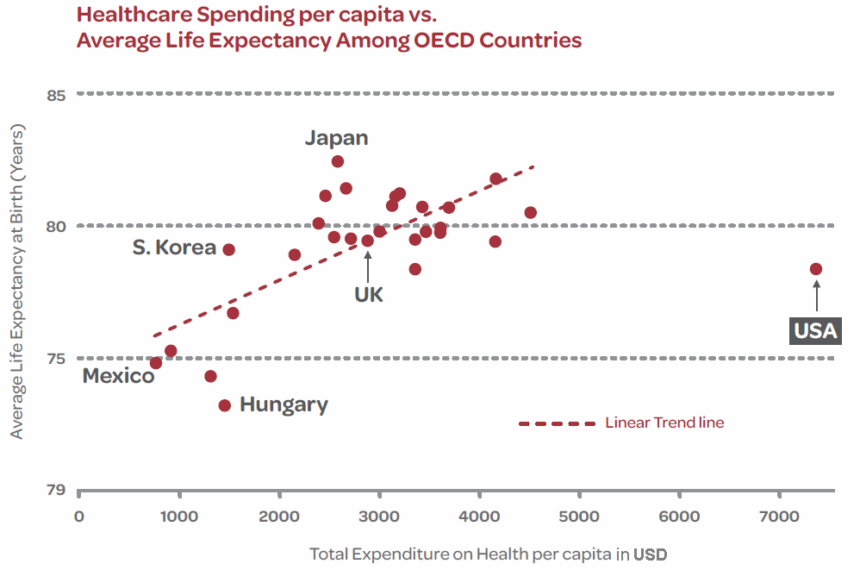
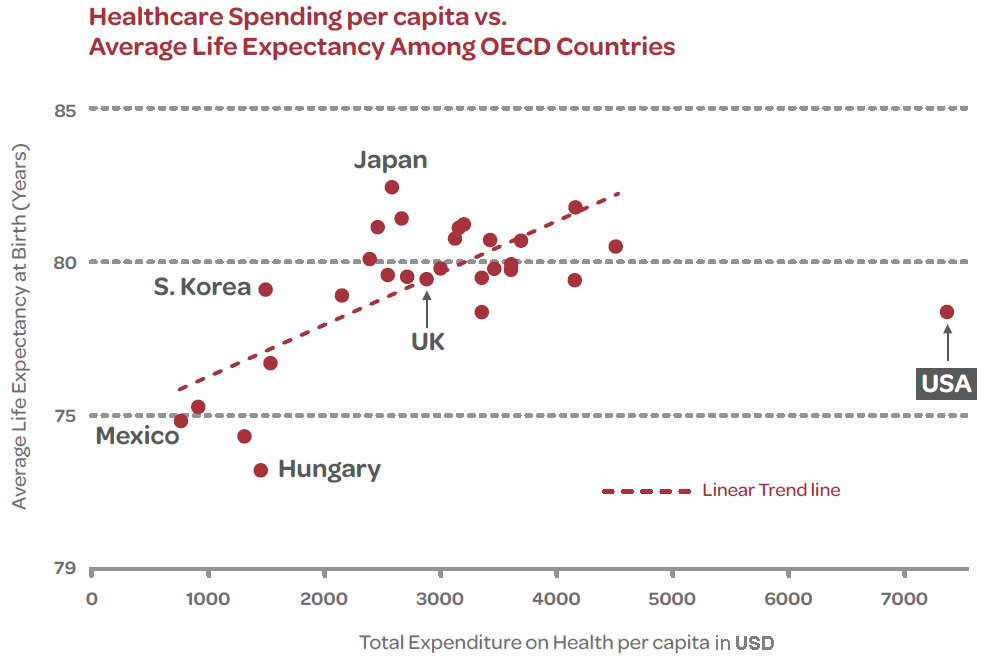
As a country, we’ve completely succumbed to the well publicized fact that our healthcare system is officially the most expensive in the world. It’s often more expensive by a factor of 2 (or more) when compared to other industrialized countries on a per-capita basis. Here’s the chart based on 2009 data from the Organization for Economic Co-operation and Development (OECD):
Editor’s Note: Dan Munro is a contributing editor to Forbes.com. His columns are collected under the heading, “The HealthCare Compass.”
As a country, we’ve completely succumbed to the well publicized fact that our healthcare system is officially the most expensive in the world. It’s often more expensive by a factor of 2 (or more) when compared to other industrialized countries on a per-capita basis. Here’s the chart based on 2009 data from the Organization for Economic Co-operation and Development (OECD):
At $3 trillion per year – our National Healthcare Expenditure (NHE) is more than the entire GDP of basically every other country on the planet – except 3 – China, Japan and Germany. We will likely surpass Germany’s GDP (~$3.5 trillion) by 2015 – if not sooner. The source of GDP data makes no difference either because the fact remains across all four of the leading sources for 2011 GDP data. That includes the United Nations, The International Monetary Fund, the CIA World Factbook and the World Bank.
It’s simply a given. No dispute. No debate. Fair enough. So what’s left to debate if you’re King of the Healthcare Pricing World? How about quality. Two of the most common benchmarks globally are Life Expectancy (U.S. world rank #37) and Infant Mortality (U.S. world rank #34). Not surprisingly, the data that supports those rankings is often disputed. Today’s report on the safety of American Hospitals by The Leapfrog Group (an employer-backed non-profit) is equally contentious. As reported by the L.A. Times:
Of the 2,618 hospitals across the U.S. reviewed by Leapfrog:
- 56% (1,468) were given an A or B
- 38% (1,004) were given a C
- 6% (146) were given a D or F
Basically, 44% of the hospitals reviewed were given a C, D or F. One of the nation’s more respected and well known healthcare institutions – UCLA Medical Center – received an outright F. In an effort to give hospitals time to boost sagging grades, Leapfrog withheld their finding for UCLA from an earlier version of their report card in June. Clearly the additional time didn’t help. As is so typical of this type of data, the Chief Medical Officer at UCLA vehemently denied the assessment and blamed it entirely on Leapfrog’s reporting methodology. Other hospital organizations also criticized the findings. From the L.A. Times article:
“UCLA is not an F hospital in quality and safety. It is not a fair scoring system and it does a disservice to the public.” Tom Rosenthal, Chief Medical Officer at Ronald Reagan UCLA Medical Center
So who’s right – and how do we as consumers (and ultimately patients) know? We don’t. What we do know is that the entire industry spends a great deal of time, energy and effort arguing over data. It often starts – as Hugo Campos found out – with who owns the raw data itself. In Hugo’s case, the headline highlights the dilemma: Should Patients Have Access to Implant Data? Medtronic, Boston Sci Weigh In.
Say what? Med device companies get to “weigh-in” on who owns the data their devices are recording – inside a patient? At what point did we lose the sovereignty of our own beating heart? It’s actually quite easy to answer that one. Clearly we never had it – so the fight (led by patients like Hugo) is to get it back.
That data battle continues on the clinical side as well. From an article I wrote in August – Healthcare’s Question of the Decade:
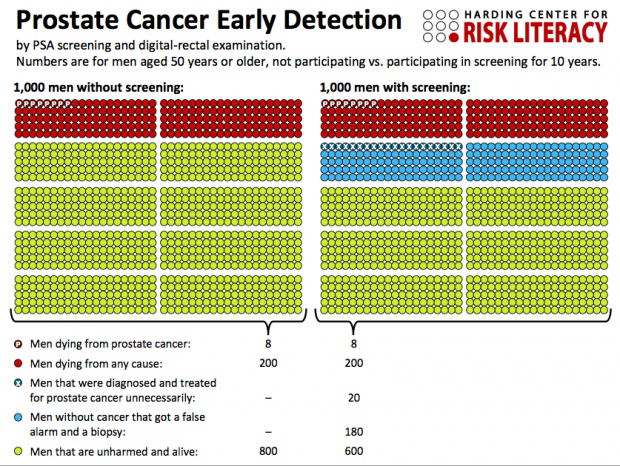
For years we’ve been sold on the clinical benefits of things like PSA Screening, Hormone Replacement Therapy, Colonoscopies and Mamograms. Over the last decade, millions of these clinical tests have been done – but the clinical evidence to support their benefit wasn’t only missing – in many cases these procedures often resulted in more harm than good. Here’s the chart that highlights the results of several studies:
In May of this year, the U.S. Preventative Services Task Force (USPSTF) gave PSA Screening a ‘D’ recommendation. [Grade D. The Task Force recommends against this service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits.] Needless to say, many urologists strongly opposed the revised recommendation and the American Urological Association was quick to highlight their “outrage.” I had one urologist post a dissenting opinion on the article I wrote in August.
Just last week, the USPTF came out in favor of HIV screening for all patients age 15-65 and pregnant women – regardless of risk. The clinical rebuttal – The Case Against Universal HIV Screening – appeared the same day.
Healthcare pricing transparency is only a fractional first step on our way out of this wilderness. The financial data itself is also getting much easier to find. WalMart publishes their list of $4 prescriptions here. The Surgery Center of Oklahoma publishes their cash price online here. The one caveat?
NOTE: If you are scheduled for surgery at our facility and we are filing insurance for you, the following prices do not apply to you.
The real challenge ahead isn’t as much about pricing itself – as value. That remains the real mystery – and where we’ll continue to see strong resistance against real accountability. Paul Keckley – Executive Director, Deloitte Center for Health Solutions – said it best:
“It’s a dicey issue because on the one hand physicians expect high compensation based on their years of training and clinical expertise, but on the other hand they can resist efforts to provide data about their performance – report cards if you will.”
We need a lot more than just pricing transparency in healthcare. We need industry transparency. Report cards like the one just released today by Leapfrog are just what the patient needs – even if the Chief Medical Officer didn’t order it.