Cancer affects many people around the world, casting a dark shadow over their lives. Detecting cancer early and diagnosing it accurately are really important for successful treatment. Advanced imaging, like PET scans and MRIs, has changed the game in this fight against cancer. These imaging techniques give us detailed pictures of what’s happening inside the body, helping doctors understand the battleground where cancer is fighting.
But, like any big change, using these advanced imaging techniques also brings challenges. We need to carefully understand how to use this new technology responsibly.
Revolutionizing Diagnosis
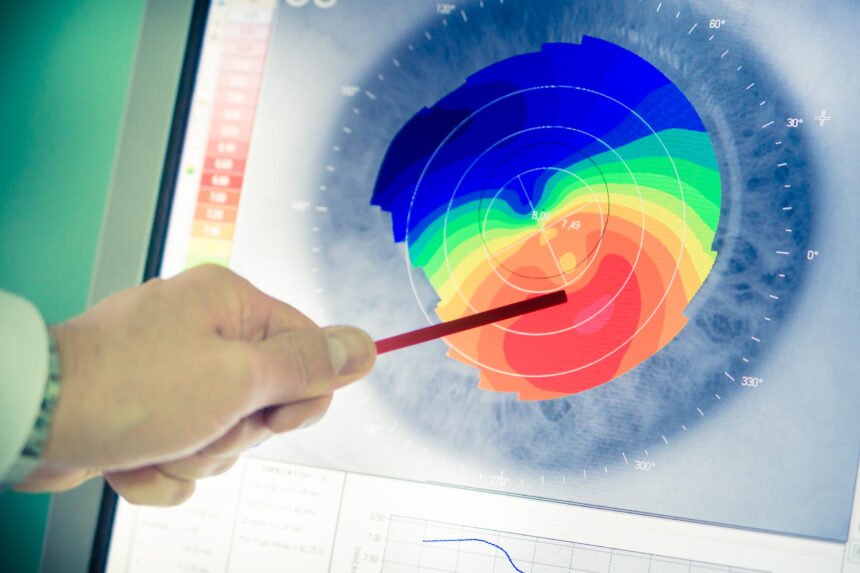
There are different types of imaging techniques. PET scans show us where there’s a lot of metabolic activity, which can help find hidden tumors because tumors often use a lot of sugar. CT scans give us a detailed look at the body’s anatomy, showing the size and location of tumors. MRIs give us clear images of soft tissues, helping doctors figure out what kind of tumor it is and if it’s spreading. Along with other techniques like ultrasound and biopsy, these imaging methods give doctors a lot of information to make decisions about diagnosis, how far the cancer has spread, and what treatment to use.
Using these advanced imaging techniques has made a big difference. Finding cancer early because of these images means treatments work better. Imagine finding a tumor when it’s just starting to grow, before it spreads too much. These imaging techniques give us that chance, leading to more people surviving cancer and having a better quality of life. Also, knowing more about the tumor helps doctors create personalized treatment plans, making sure the treatment works well and has fewer side effects.
Emerging Challenges
However, just like a complex DNA strand, this revolution in cancer diagnosis has its own set of challenges that need careful consideration. These advanced imaging techniques provide a lot of information, but sometimes this wealth of data can be a double-edged sword. Small details, unclear results, or the absence of clear markers can create confusion and mistakes in interpretation, leading to unnecessary procedures and anxiety for patients. For example, if a PET scan shows something unclear, it might prompt a biopsy that wasn’t really needed, causing stress and potential complications.
Balancing Accuracy and Responsibility
To tackle this challenge, doctors need to balance the information from the images with other important factors like a patient’s medical history, physical exams, and lab results. Working together in teams that include radiologists, oncologists, and other specialists is crucial for solving complex cases and making the most accurate diagnoses.
There are also legal considerations to keep in mind. According to a lawyer specializing in cancer misdiagnosis, making mistakes in interpreting imaging data, especially if it leads to a misdiagnosis, can result in lawsuits. Following established medical standards and protocols is essential to make sure these powerful tools are used responsibly. A skilled cancer lawyer can provide the necessary legal guidance to navigate the complexities of such cases with expertise and compassion.
Advanced Imaging is Still Growing
It’s important to recognize that this journey is ongoing. Medical imaging technology keeps improving, and new developments in artificial intelligence (AI) are promising to help analyze data more accurately and reduce mistakes in interpretation. Also, personalized medicine, which uses genetic and molecular information, is leading to more targeted imaging methods, making diagnoses and treatment plans even more precise.
In the end, the story of advanced imaging in cancer diagnosis isn’t just about the technology itself, but about how we use it responsibly and wisely. By acknowledging the challenges and successes of this revolution, we can work towards a future where these advancements truly make a difference in the lives of people fighting cancer. This means using these tools responsibly, always learning and improving, and working together to prioritize the well-being of patients above all else. This way, we can truly transform how cancer is diagnosed and treated, bringing hope and healing to many.