Most of the people I meet in my voyages ’round healthcare system transformation, grassroots edition, arrived at the portal of #epatient via a trip through the medical-industrial complex. Either they, or someone they cared for, wound up getting “a thing” – cancer, Parkinson’s, multiple sclerosis, player to be named later – and they found themselves inside the medical care delivery system, bewildered, and looking for answers. In short, most – not all, by any means, but most – are over 40.
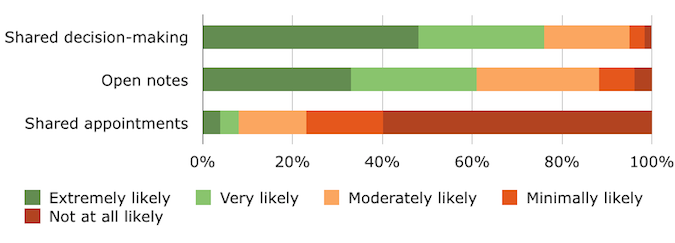
Most of the people I meet in my voyages ’round healthcare system transformation, grassroots edition, arrived at the portal of #epatient via a trip through the medical-industrial complex. Either they, or someone they cared for, wound up getting “a thing” – cancer, Parkinson’s, multiple sclerosis, player to be named later – and they found themselves inside the medical care delivery system, bewildered, and looking for answers. In short, most – not all, by any means, but most – are over 40. Imagine my surprise, and delight, when I was sent a report on a survey conducted with 385 randomly selected patients across the US*, with most of the responses coming from 18 to 35 year old millennials (people born 1982 and after). The survey asked them their opinions on shared decision making, open notes, and shared medical visits, three new medical practice models that are rising in adoption. Here’s the context of the survey questions:
- Shared decision-making involves the doctor and patient evaluating multiple treatment options and deciding together on the best course of action.
- Open notes is a policy allowing patients to view the medical notes doctors take about them during visits, which includes accessing those notes from home.
- Shared medical appointments, or “group visits,” involve attending an extended (60- to 90-minute) medical appointment with 10 to 15 other patients and one or more physicians.
The survey results make me think we might finally be reaching a tipping point toward positive change, given that a big majority (76%) of respondents said they were extremely or very likely to use shared decision making. Over 60% were extremely or very likely to welcome open notes: 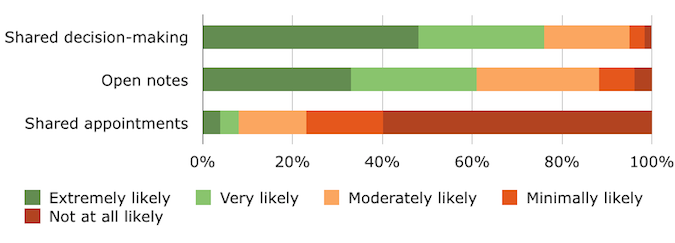 The demographics of the survey respondents was a pretty representative sample as far as chronic conditions go:
The demographics of the survey respondents was a pretty representative sample as far as chronic conditions go: 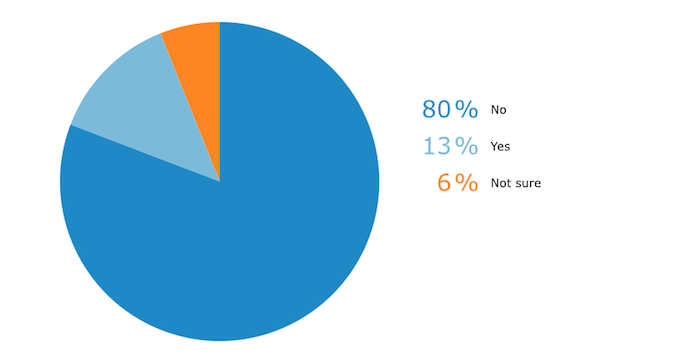 One surprise in the demographic detail was that more men responded than women. Given that, historically at least, women have been more likely to use the medical care system (annual Pap smears, reproductive health visits) than men, the fact that men outnumbered women in this gives me even more hope. Are dudes getting it? “It” being that their health is their responsibility, and that a relationship with a good primary care provider is a good life plan.
One surprise in the demographic detail was that more men responded than women. Given that, historically at least, women have been more likely to use the medical care system (annual Pap smears, reproductive health visits) than men, the fact that men outnumbered women in this gives me even more hope. Are dudes getting it? “It” being that their health is their responsibility, and that a relationship with a good primary care provider is a good life plan. 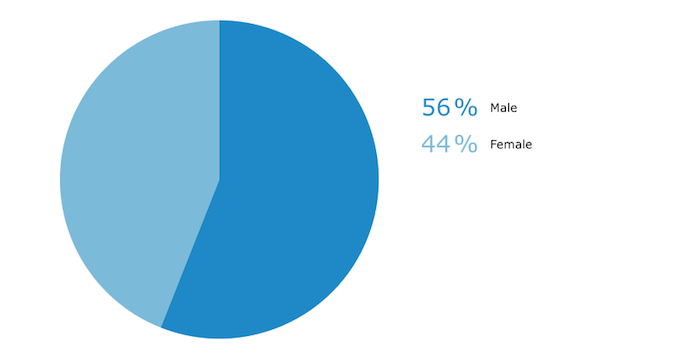 To recap, millennials want shared decision making and open notes. Shared/group appointments, not so much. I think that the shared/group appointment approach would be best deployed in “building health literacy” settings: condition-specific education on diabetes, for example. I also think that telemedicine needs its own survey, given that practice model could be used both real-time or asynchronously via secure video links. The millennial generation has grown up with digital tools and instant access to information. I seriously doubt that they’re going to be willing to suffer the slings and arrows of outrageous wait times, or outrageous balance billing, when they seek medical care. Hope for real system transformation may have crested the distant horizon, and be riding toward us. May its speed be supersonic.
To recap, millennials want shared decision making and open notes. Shared/group appointments, not so much. I think that the shared/group appointment approach would be best deployed in “building health literacy” settings: condition-specific education on diabetes, for example. I also think that telemedicine needs its own survey, given that practice model could be used both real-time or asynchronously via secure video links. The millennial generation has grown up with digital tools and instant access to information. I seriously doubt that they’re going to be willing to suffer the slings and arrows of outrageous wait times, or outrageous balance billing, when they seek medical care. Hope for real system transformation may have crested the distant horizon, and be riding toward us. May its speed be supersonic.