Have you been to the emergency room lately? Everyone tries to avoid ERs. For one thing they are meant for emergencies, and despite that fact there are many who use the ER in the evening on the weekends and holidays when their doctor is not available. This is especially true if you see a physician in a small group or a solo practitioner. Many sign out to the ER, and because ERs must examine all comers (by law) these patients add to the constant stream. Some arrive at the ER from an accident, some have no physician at all. Wait times are variable The frequency of true emergencies is very small. Triage is critical, and in some cases there is an urgent care center nearby that a patient can be referred to.. In our particular hospital there is a common reception area and a nurse practitioner or physician assistant screens a patient and refers them left to urgent care or right to the emergency department. Any chest pains are immediately shunted to the vital signs room to be hooked up to monitors, have blood drawn and have a detailed history taken.
The topic of my blog is not about triage and treatment in the emergency room but how ED visits are billed in general. This was brought to mind when I received a MedThe icare Summary Notice from 18 months prior to receiving the notice. It speaks loudly about problems which simmer and simmer but never seem to be addressed.
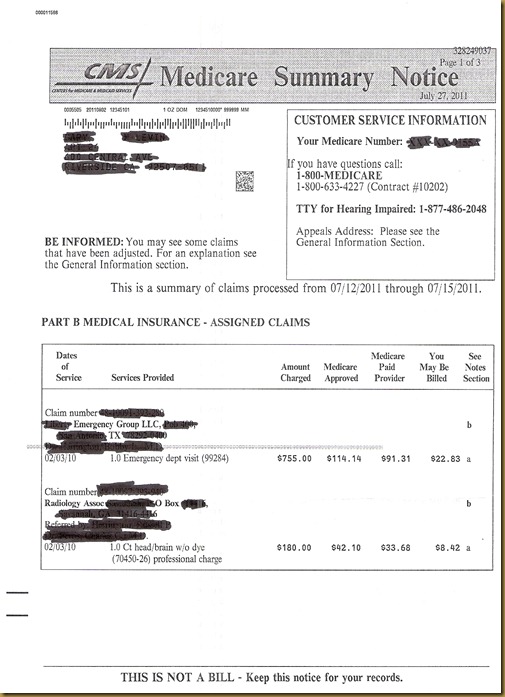
The notice :
This is a typical Medicare Summary Notice which Beneficiaries receive in a month where their CMS has been billed:
1. Please notice the date of the notice: upper right corner: July 27, 2011. It arrived in my snail mail box on August 12, 2011.
2. Notice the Date of Service: 02/03/2010, the ED location was in a small town in Georgia.
3. Notice the billing address is in Texas.
4, The providers were from an ED group (not the radiologist however).This is not uncommon because many EDs are staffed by companies that provide ED doctors for an entire region or part of one.
5.The total amounts billed to Medicare were $ 755.00 and $ 180.00, while the Medicare approved amounts were: $ 114.14 and $ 42.10, and the CMS payments were: $ 91.31 and $ 33.68. The remaining balance that I ‘might be billed’ was $ 22.83 and $ 8.42 .
Had I not had insurance, or Medicare I would have been billed the totals amounts of $ 755.00 + $ 180.00. The hospital might have given me a cash discount if I asked, however they would not volunteer that information.
The questions arise:
1. Why did it take 19 months for me to receive a summary notice? You will notice the claim was processed between July 12-15 2011. Was the bill sent in 16 mos late? CMS usually pays an electronic claim within 14-21 days. Why did it take the providers 16 mos to submit their charges to CMS. Imagine if you will what their accounts receivable must look like.
2. Should I be euphoric that the bill was for $ 935.00 and I only would get billed: $ 31.25
3. No one can really construct a logical reason why the amount billed, the amount allowed and the amount paid are so disparate. It must be the law combined with an attempt to show immense billings as a measure of importance for that hospital in a chain.
Not many people plan to go to the ED, but there are some who do. Drug dependence is one area where patients make elective visits to the ED. There are not that many choices in picking an ED, so price comparisons don’t play a big role in selecting an emergency department.
I’ve been a physician for 40 years, and this was going on when I started practicing, so it is nothing new…
Akron General Patient Price Information Emergency Department
Demystifying, and Maybe Decreasing the Emergency Room Bill
Consumer Health Ratings: Typical Average Cost of Hospital ED Visit