Folks must think that all doctors know all things medical. I know this is true by the questions that I have been asked over the years. While my expertise spans from hemorrhoids to heartburn, I am routinely queried on medical issues well beyond the specialty of gastroenterology. When I can’t answer questions about a new medicine for hypertension or if an MRI of the shoulder makes sense, folks look at me quizzically as if I must not be a real doctor.
Folks must think that all doctors know all things medical. I know this is true by the questions that I have been asked over the years. While my expertise spans from hemorrhoids to heartburn, I am routinely queried on medical issues well beyond the specialty of gastroenterology. When I can’t answer questions about a new medicine for hypertension or if an MRI of the shoulder makes sense, folks look at me quizzically as if I must not be a real doctor.
Today, more than ever, physicians are highly specialized with a very narrow medical niche. There are ophthalmologists, for example, who only treat retinal disease. Perhaps there are even retinal specialists for the left eye only. It wouldn’t surprise me.
My partners and I perform routine gastroenterology procedures in an ambulatory surgery center. Patient safety is our priority and our staff and us are dedicated to this mission. All of us are required to be certified in Advanced Cardiac Life Support in the unlikely event that a medical urgency develops. We recertify every two years, and recently did so.
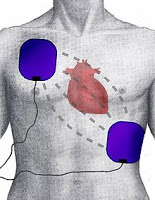
Defibrillation
Ordinary readers will view this requirement as sensible. Physicians who perform procedures should be conversant with advanced life support measures including defibrillation and cardiopulmonary emergencies. At our recent recertification, an experienced paramedic spent 4 hours in our office transferring ACLS knowledge to us and pointing out all of the new doctrine that had developed in the past two years. In other words, the stuff from two years ago that we had long forgotten was no longer operative. At the conclusion of the session, we all passed the recertification examination.
Does this really make sense? Physicians understand that clinical skill depends upon case volume. Indeed, medical research has confirmed that physicians and institutions that perform surgeries and procedures more often do so with greater skill and fewer complications. While volume is not the only consideration when choosing a surgeon, one who does the operation regularly has a clear edge.
How often do gastroenterologists like me practice ACLS? Never. The only time this is on my agenda is every two years when I must recertify. In the interim, I don’t read about it, witness it or practice it. This is why ACLS should be performed by professionals who are in the ACLS arena regularly. Should a physician who hasn’t been responsible for reading electrocardiograms (EKGs) for decades, be asked to interpret complex heart rhythm disturbances on the spot and then know immediately what the treatment should be? This is absurd and we know it.
ACLS is not just performing chest compressions and mouth-to-mouth resuscitation, skills that should be known by everyone. (Note that the latter feature of basic life support [BLS] has been
revised by the American Heart Assocation.)
ACLS is a complex specialty requiring deep knowledge and regular exposure if its practitioners are to remain sharp. Gastroenterologists need not apply. Leave it to the professionals.