Over the last few months, H7N9 has been making headlines around the world. As of May 9, there have been 130 identified cases. 31 of them have died and 42 of them have recovered. Fortunately, H7N9, with a fatality rate of over 20 percent, has not spread to regions outside of greater China (all identified cases were in mainland China and Taiwan). The number new cases seems also decreasing as the temperature rises and a large scale outbreak is not likely at this point.
We may have survived another flu season.
Over the last few months, H7N9 has been making headlines around the world. As of May 9, there have been 130 identified cases. 31 of them have died and 42 of them have recovered. Fortunately, H7N9, with a fatality rate of over 20 percent, has not spread to regions outside of greater China (all identified cases were in mainland China and Taiwan). The number new cases seems also decreasing as the temperature rises and a large scale outbreak is not likely at this point.
We may have survived another flu season.

A woman wears a face mask as she walks past a poster that reads “Facing H7N9: Be Aware; Don’t Panic.” (Photo: AFP)
Epidemiologists pointed out that new pathogens of infectious diseases like influenza have posed new challenges to public health. Ten years after the SARS outbreak, the H7N9 pandemic once again reminds us new pathogens can be highly fatal. Comprehensive preparedness for public health crisis is crucial to contain massive transmission among humans, identify pathway of the disease and find effective treatments in the early stage of a pandemic.
There are four things we should learn from responses to H7N9, which have so far led to effective control of the disease.
Immediate response and transparency is key to contain transmission at early stage.
The first H7N9 case was identified on March 31 and it was then quickly announced in both local and national media outlets. The relatively prompt reaction played an important role in raising people’s awareness of the disease. As a result, preventative steps (e.g., shutting down live poultry markets and avoiding close contact with live birds) may have reduced the infection. This is a big improvement compared to how the government handled SARS, in which case it hid the numbers from WHO and media until hundreds of people were sick and a larger outbreak became inevitable.
Communication regarding the N7N9 infection cases and deaths has been transparent during the course of the outbreak. Indeed, it is nerve-racking to see the high fatality of the disease, but the numbers have also helped to put the outbreak in perspective, informing the general public that the outbreak is sporadic and there is no need to panic.
Preparedness for pandemics is crucial.

It was a painful lesson for China to learn from SARS 10 years ago (Photo: AFP)
A painful lesson the Chinese government learned from SARS is that the country was ill-prepared for acute infectious diseases. The building of public health infrastructures was much behind the country’s overall urbanization progress. With millions of people moving into cities from rural countryside, the fragile public health facilities in some cities almost collapsed when SARS hit. Meanwhile, a lack of experience in dealing with large-scale disease outbreaks resulted in a series problems that caused more lives– inefficient use of existing public health resources, avoidable infections in hospitals, slow responses from academia and low public health literacy among the general public.
A decade later, measures taken after SARS show how some of the improvements have helped highly populated cities to better deal with a dangerous disease outbreak.
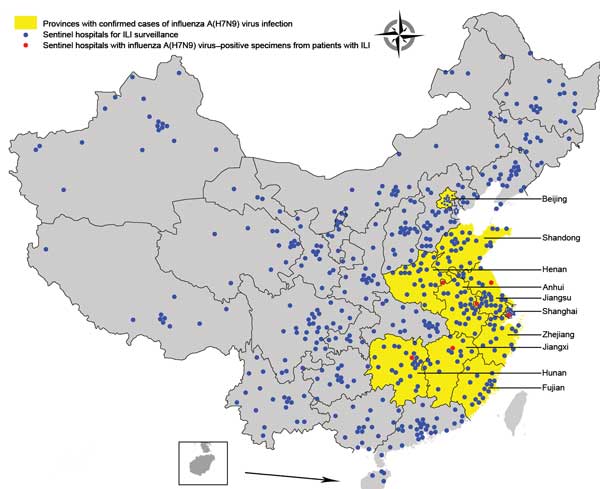
Geographic distribution of national influenza surveillance sentinel hospitals in Beijing and Shanghai Municipalities and 8 provinces with confirmed human cases of avian influenza A(H7N9) virus infection, China, 2013. (Photo: CDC)
According to the CDC of China, The country has established two major infectious disease monitoring and reporting networks—SARS Surveillance System and China National Major Infectious Diseases Surveillance System. During the H7N9 outbreak, the Ministry of Health was able to receive prompt updates directly from each province major cities. China Radio International reports that by April 8, China CDC had distributed more than 160,000 testing kits via its network that covers all labs in the country’s 31 provinces.
A group of Chinese scientists in early April published a study in Emerging Infectious Diseases, a journal published by the CDC. The study highlights the important role of Chinese National Influenza-Like Illness Surveillance Network (which was created after the H7N9 outbreak) in identifying new cases and facilitating epidemiology studies of the disease.
Share information with international counterparts.
From SARS to H5N1, we have seen how a local outbreak can flare into a global crisis. Sharing information with WHO and other countries is a necessary step to avoid an outbreak on the global level. Additionally, sharing information also expedite the process of understanding the disease and finding effective treatments.
Soon after the H7N9 virus was identified, it was sent to major labs in the U.S. and the U.K. Virologists have since worked collectively to solve mysteries surrounding H7N9, hoping to develop a vaccine.
On April 24, Chinese scientists also published a study in NEJM, analyzing the epidemiological characteristics of H7N9 and discussing how the virus changes after infecting human bodies.
As I mentioned in an earlier blog post, as significant changes have occurred in the environment we live in, new diseases are real threats to the modern society. Although H7N9 may be losing its momentum, people in public health need to stay on high alert.