Just back from the American Telemedicine Conference, and we took a short trip over the border (and back
Just back from the American Telemedicine Conference, and we took a short trip over the border (and back
 Just back from the American Telemedicine Conference, and we took a short trip over the border (and back to the motherland), to the Canadian E-Health Conference in Vancouver, BC. Due to the short timeframe between conferences, it’s hard not to compare and contrast the two, although the healthcare systems between Canada and the US could not be more different. The E-health conference had a broader scope than the ATA conference, with telehealth as a sub-topic and electronic records management featured more broadly, in fact, all the major EMR vendors were there, with the exception of Epic.
Just back from the American Telemedicine Conference, and we took a short trip over the border (and back to the motherland), to the Canadian E-Health Conference in Vancouver, BC. Due to the short timeframe between conferences, it’s hard not to compare and contrast the two, although the healthcare systems between Canada and the US could not be more different. The E-health conference had a broader scope than the ATA conference, with telehealth as a sub-topic and electronic records management featured more broadly, in fact, all the major EMR vendors were there, with the exception of Epic.
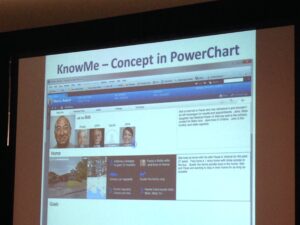
In a session sponsored by Cerner, Island Health CMIO and Acting Executive Medical Director, Dr. Mary-Lyn Fyfe shared their patient-centered approach to EMR implementation called “Know Me.” Island Health Authority has been a Cerner customer for 5 years, and have a robust implementation with plans to extend to patient recorded profiles. Dr. Fyfe talked about how what is most important to patients is not always evident or even apparent to healthcare providers, for example, a patient admitted for heart issues but who is more concerned about who will care for his spouse at home with dementia rather than his own condition. Only by treating the whole patient does Dr. Fyfe believe that healthcare providers can have real impact.
Although telehealth was not more advanced in Canada than what we’ve observed in the US, Canada has real financial incentives for telehealth. Vast distances and sparce populations make delivering a high-level of care in many parts of Canada very expensive. The more that can be done remotely, the better. One group covering First Nations groups boasted that they had delivered nine telebabies, that is babies delivered with the help of a doctor over telemedicine. Another doctor talked about how his being able to coach a medical assistant onsite through a video call prevented a $10,000 emergency helicopter flight. Others talked about the environmental benefits of thousands of car trips of 3-4 hours that were avoided by using telemedicine, not to mention the quality of life improvements for patients. Another benefit of telemedicine that we hadn’t seen cited before was doctor education, this is in the scenario where a local primary care physician calls a specialist and together they meet with a patient. In an in-person specialist care scenario the patient would not see these two physicians at the same time. Having both in the same patient visit enables knowledge sharing between the doctors, for the specialist more context on the patient, and for the primary care physician education about the specialist’s area of expertise and the patient’s condition. You could call this collaborative telemedicine.
While telemedicine is well established in Northern Canada, it seemed that the benefits in parts of Canada closer to the US border where most of the population lives were not as well established, and a surprising number of telemedicine initiatives were still in pilot mode. Similarly there seemed to be a great disparity in electronic records management with some health authorities still entirely on paper.
Kicking off the Canadian Telehealth Forum, which was a pre-conference session and also an annual event, Joseph Cafazzo of the Center for Global E-Health Innovation showed examples of home monitoring technology that did not take into account the users, who are primarily seniors, and called on the audience to consider empathy in the design of products. One of the key reasons for this is that the only person capable of managing a chronic illness is the patient themselves, and yet many don’t want to identify with their illness or be reminded that they have it. Empathy to the patients experience can help in designing products that make it less intrusive for patients to manage their health. The Juvenile Diabetes Foundation has been putting pressure on manufacturers for this as teens in particular don’t want to take their blood sugar readings although it’s crucial to their health. The Center for E-Health developed an application that identified the times that teens really don’t want to take readings (at lunch when they are at school for example), and offered rewards like iTunes giftcards for doing so, a great example of a carrot that is attuned to the patient’s preferences.
Mobile health seemed in the same place as in the US: a lot of very interesting, patient-centered applications like the 30-day stroke assessment from the Center for E-Health and the Heart & Stroke Foundation of Canada, which used AirMiles rewards to entice a high-risk group of men to download and complete the assessment. Engagement was 12% across all groups, including seniors. One of they keys to the app was that it focused on a short-timeframe, although this does bring up the question of how to keep patients engaged over the long-run.
Not surprisingly a number of solutions were based on lowering costs of population health management. Because healthcare is government funded, unlike the US there are real incentives for decreasing costs as well as keeping the population out of long-term care. While many solutions addressing issues such as CHF and COPD are in early stages, we heard lofty goals of increasing the number of outpatients managed by one nurse to over 200, and also using wellness coaches to scale further.
Considering that unlike the US, all the economic and patient incentives are aligned for e-health, it was a bit surprising that so many of the solutions and presentations were about pilots rather than completely implemented systems. However, that might be a tradeoff of having government run programs. Regardless, the conference featured many passionate speakers who are using innovative solutions to both improve patient outcomes and experience while being cost-effective.