Another hospital system has announced job cuts. This time, it was Baystate Health System, which announced a reduction of 354 jobs, or 3.5% of its payroll. The Boston Globe article describes the hospital suffering a $25m shortfall, blamed on lowered state Medicaid support.
Another hospital system has announced job cuts. This time, it was Baystate Health System, which announced a reduction of 354 jobs, or 3.5% of its payroll. The Boston Globe article describes the hospital suffering a $25m shortfall, blamed on lowered state Medicaid support.
Only 169 of the quoted 354 jobs involve flesh-and-blood layoffs, with the balance coming from the elimination of open positions. Baystate is the latest in a series of medical centers that have trimmed positions in the 3% range. Each center faces common challenges from the changes likely to come under health reform, but these are superimposed upon the environment particular to the individual entities.
Having spent five tough, but ultimately rewarding years at this particular medical center, I can speculate on two of the issues likely facing Baystate. The first item is probably more significant, though both are challenging to tackle.
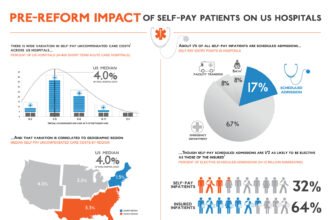
1) Difficult demographics: Baystate is located in the Hampden County city of Springfield, tucked out in western Massachusetts. Its a classic New England locale, but the surrounding population’s economic profile is lower than the rest of the state by a significant margin. The article notes that 26% of the patients are on Medicaid. I would term that as accurate or possibly even a low estimate. According to 2010 data, 17.2% of the county is below the poverty level, which is almost 7% more than the state average. Per capita and household incomes are both about 27% lower than the state average. This means that the hospital’s fortunes are tied greatly to what happens to Medicaid funding, and right now that funding is under pressure until (and if) it is raised under health reform
2) Patient Drain: There is some drain of area patients to centers in Boston, and occasionally Worcester. I don’t have exact data, and this phenomenon is not unique to Massachusetts. But the effect is probably worse in smaller states. A 90 minute ride to Boston is far easier than a midwesterner driving 10 hours to the Mayo Clinic. There isn’t good evidence that these centers provide better care except for exotic services that only they provide. Baystate can do almost (but not quite) everything that Boston can. It’s a good idea to identify the routine services leaving the area and work on keeping that care local. Also, those leaving the area for care likely are well insured, and hail from the affluent suburbs.
On the plus side, Baystate is the flagship hospital for the region, and is affiliated with an academic medical center. It draws from most of the area including the border areas with New York, Vermont, and Connecticut. It has been well managed and has not been subjected to large financial shocks.
Hospitals can’t do much about regional demographics, and influencing Medicaid funding is difficult. Managers are thus focusing on the levers that are under their control, namely operations and payroll. But the challenges faced by hospitals such as Baystate are just a prelude to what may be required once the effects of the health reform legislation start to unfold.